Breast cancer is the most frequent cancer type among women. According to the World Health Organization, it is estimated that in 2018, 627,000 women succumbed to the disease. The progression of breast cancer is orchestrated by a multitude of cell types and their released factors. In fact, in addition to the breast cancer cells themselves, non-cancer cell populations found in the tumor play critical roles in the course of the disease. These non-cancerous cells constitute the breast tumor microenvironment and include mammary cancer-associated fibroblasts (CAFs), blood vessel cells, and various immune cell populations.
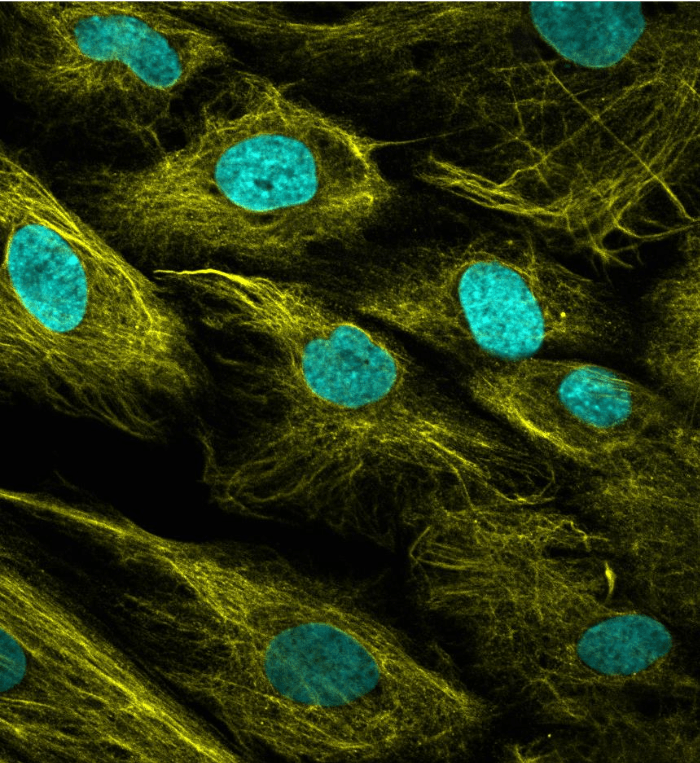
CAFs are an abundant cell population in breast tumors and are typically in contact with the tumor vasculature. CAFs have the exceptional ability to remodel their surrounding environment and signal to adjacent cells. They secrete a plethora of soluble factors and extracellular matrix components, which can alter the behavior of the surrounding cells. Depending on the context, CAFs-secreted factors can either promote or restrain cancer progression.
Blood vessels provide oxygen and nutrients that sustain the uncontrolled growth of tumors and serve as a route for cancer cells to spread throughout the body to form metastases at secondary sites. The rapid expansion of tumors is accompanied by the development of an intratumoral vascular network. However, these blood vessels are structurally and functionally abnormal, causing the formation of hypoxic (low oxygen) or completely anoxic (no oxygen) regions within the tumor. In an attempt to restore the oxygen and nutrient supply, cancerous and non-cancerous cells secrete factors to promote the recruitment of new blood vessels, a process that is termed angiogenesis.
The most potent known pro-angiogenic factor is the vascular endothelial growth factor A, or VEGFA, which is abundantly produced and secreted by cells exposed to low oxygen tension. In addition to VEGFA, hypoxic cells have also been reported to secrete a multitude of other pro-angiogenic proteins. This exacerbated pro-angiogenic signaling causes the formation of a dysfunctional and compromised vasculature, which in turn enhances the formation of hypoxic regions within the tumor, creating a vicious cycle between hypoxia and dysfunctional blood vessels. This vicious cycle is difficult to break and has a direct impact on the efficacy of response to chemo and radiation therapies.
Chemotherapeutic drugs reach the tumor via blood vessels, and when the vasculature of the tumor is compromised, these drugs can no longer efficiently penetrate the tumor to perform their cancer-killing function. Likewise, radiation therapy requires the presence of oxygen to be effective, when the vascular network is not functional and hypoxia takes place, the response to radiation therapy is impaired. Therefore, the development of efficient strategies able to reprogram the vasculature of tumors from a chaotic to a functional state, a process called vessel normalization, will be beneficial to the response of patients to existing cancer therapies. We reasoned that a deeper understanding of how CAFs shape angiogenesis in the context of hypoxia could provide valuable insights in how the tumor microenvironment contributes to the formation of a dysfunctional vasculature and potentially provide microenvironmental targets for vessel normalization.
The aim of our study was to understand how mammary CAFs exposed to low oxygen levels influence angiogenesis. We exploited an unbiased Stable Isotope Labeling with Amino acids in Cell culture (SILAC)-based mass spectrometry (MS) proteomics approach. This technology accurately measures the levels of thousands of proteins, and allow determining which proteins increase levels and which ones decreased levels when CAFs are exposed to hypoxia. Our data shows that the levels of hundreds of proteins were regulated by hypoxia in CAFs.
Notably, we found that hypoxia remodels the proteome and secretome of CAFs to promote angiogenesis. Under low oxygen tension, CAFs secrete higher levels of a multitude of known pro-angiogenic proteins, including VEGFA, Stanniocalcin-1, Lysyl Oxidase-Like 2, C-X-C motif chemokine 12, Annexins 1 and 2, and collagen 6-α. Moreover, we observed a decrease in the levels of collagens that give rise to the anti-angiogenic fragments vastatin, arresten, and canstatin. Taken together, our findings show that hypoxic CAFs tip the balance toward an angiogenesis-promoting state. Therefore, mammary CAFs exposed to hypoxia can contribute to the formation of a dysfunctional vasculature typical of aggressive tumors.
We also discovered that the protein mostly induced by hypoxia in CAFs was an uncharacterized protein called NCBP2-AS2. In breast cancer patient tissues, we observed that NCBP2-AS2 was expressed in the tumor microenvironment of a subset of breast cancer patients and that its frequency was increased with the progression of the disease. Strikingly, the silencing of NCBP2-AS2 in hypoxic CAFs significantly decreased their ability to promote angiogenesis, using models of vessel capillary growth in a three-dimensional matrix in vitro and measuring the vessel density in mice in vivo.
To shed light into the molecular mechanism behind the pro-angiogenic function of NCBP2-AS2, we again used an unbiased MS-proteomics approach. We discovered that the secretion of the master angiogenesis regulator VEGFA was decreased in hypoxic CAFs when NCBP2-AS2 was silenced. In line with this finding, the decreased angiogenesis observed upon NCBP2-AS2 silencing could be rescued via VEGFA addition. Moreover, the use of the VEGFA neutralizing antibody bevacizumab did not cause additive inhibitory effect in angiogenesis upon NCBP2-AS2 silencing. Finally, the secretome of hypoxic CAFs silenced for NCBP2-AS2 had a diminished ability to activate the VEGFA downstream signaling when used to treat blood vessel cells, as measured by the phosphorylation levels of VEGFR2, PLCγ, AKT, and ERK 1/2. In light of these findings, we proposed to rename NCBP2-AS2 to HIAR: Hypoxia-Induced Angiogenesis Regulator, reflecting the functional role of this protein, discovered in our study.
In cancer patients, the efficacy of therapies targeting the vasculature has been dismal. The majority of anti-angiogenic approaches target VEGFA itself, by using neutralizing antibodies, or its receptor. However, because VEGF signaling also controls blood vessel homeostasis in physiological conditions, targeting this pathway results in unwanted side effects. The discovery that HIAR regulates VEGFA levels under hypoxia, which is associated with pathological angiogenesis, may represent a novel therapeutic avenue to disrupt the dysfunctional angiogenesis in tumors without interfering with the physiological vasculature.
These findings are described in the article entitled Hypoxic cancer–associated fibroblasts increase NCBP2-AS2/HIAR to promote endothelial sprouting through enhanced VEGF signaling, recently published in the journal Science Signaling.









