Circadian rhythms, 24-hour internal clocks running in all cells, aid living organisms in acclimatizing their physiology and behavior to the day/night changes in light, temperature, accessibility of food, and other periodic ecological factors.
The wake/sleep sequence that steers between alertness and sleepiness at consistent interludes is the best known example of circadian rhythm. Such rhythms are found on a broader spectrum of biological processes from body temperature and hormone secretion to cognition and memory. These rhythms are produced by “clock genes,” which drive the 24-hour cyclical expression of up to 50% of the entire genome.
The molecular machinery underlying this phenomenon was discovered in the mid-late 80s, and the work received a Nobel Prize in Physiology and Medicine in 2017. In mammalian species, every single cell has this clock machinery and acts as an independent oscillator that works in synchrony with other oscillating cells in a multi-oscillatory system. The master circadian clock, or the central pacemaker of circadian rhythms, is the suprachiasmatic nucleus located in the hypothalamic region of the brain. The neurons in this tiny region of the hypothalamus regularly receive photic and nonphotic inputs from the environment as well as different organs in the body to orchestrate the endogenous rhythms and synchronize them to environmental cues.
Disordered external signals, misaligned internal clocks, or alterations in the expression of clock genes are harmful to human health, as it can enhance the susceptibility and severity of many metabolic and neuropsychiatric disorders. For example, jet lag disorder, seen in individuals who quickly travel across multiple time zones or work on night shifts, is a result of lack of synchrony between the internal clock and external rhythms.
Epilepsy, the most common neurological disorder after stroke, is often medically intractable. The occurrence of unpredictable intermittent seizures exemplifies epilepsy as an outcome of imbalance in excitatory and inhibitory neurotransmission in the brain. Remarkably, the interaction between seizures and circadian rhythms occurs in a bi-directional manner. Environmental cues such as food and light can modulate both the onset and severity of seizures. The seizures also modify the temporal oscillation of several biological processes, including body temperature, locomotor activity, sleep pattern, and secretion of hormones.
A notable feature of this crosstalk is that the occurrence of seizures, though unpredictable, is rhythmic. Therefore, discerning how the circadian system and seizures influence each other is of great interest in understanding not only the pathophysiological features of epilepsy but also for developing new therapeutic strategies. This association has particularly been examined in mesial temporal lobe epilepsy (mTLE), a type of acquired epilepsy affecting >30% of epilepsy patients where seizures originate from the temporal lobe foci such as the hippocampus. Cognitive, memory, and mood impairments are the behavioral comorbidities in mTLE, which are typically associated with multiple adverse epileptogenic changes and abnormal plasticity in the hippocampus. The seizures in patients afflicted with mTLE usually peak in the early morning and/or afternoon.
A recent study demonstrated that some clock genes display dysregulated oscillations in their expression in the hippocampus of epileptic animals which can enhance the occurrence of seizures at precise time-points by affecting the 24-hour oscillations of molecules that play a role in excitatory or inhibitory neurotransmission. For instance, at night, when seizures are less frequent, high levels of melatonin and reduced activity of mammalian target of rapamycin (mTOR) are observed, which are the two crucial regulatory components involved in the modulation of seizure thresholds.
Furthermore, the changes in the expression of clock genes can cause misaligned oscillations between hippocampal neurons and other oscillators. In such a scenario, inhibitory neurotransmitters or molecules that regulate excitatory neural activity may not have their receptors expressed at the right time, or excitatory signals can reach the hippocampus at lower thresholds. Also, new molecules can gain 24-hour oscillation, which may contribute to the rhythmicity of seizures.
It has been demonstrated that ~30% of gene products present circadian oscillation only when the brain becomes epileptic. A disregulated clock system in the hippocampus of epileptic individuals likely also contributes to cognitive and mood impairments because the hippocampus is well connected with many other brain structures, including direct neural pathways to the suprachiasmatic nucleus and peripheral oscillators. The hyperactivity of neurons prevailing in the epileptic hippocampus could reset the clock in these structures, which in turn may affect the rhythmicity of several biological processes.
A growing understanding of the involvement of the circadian system in the generation and sustenance of epileptic seizures has shed novel insights for the treatment of mTLE, a condition in which seizures are drug-resistant in >35% of patients. Notably, the application of chronotherapy, which is a systematic execution of strategies that curtail seizures occurring from dysregulation or desynchronization of the circadian clock, has received significant attention.
It is conceivable that resetting the circadian rhythms in epileptic conditions by inducing changes in the molecular rhythms could be a co-adjuvant therapy in the management of epilepsy. This approach has been successful in treating individuals having disordered wake/sleep cycles from jet-lag or night-shift work, or with other conditions such as hypertension, immune disorders, mood dysfunction, and aging.
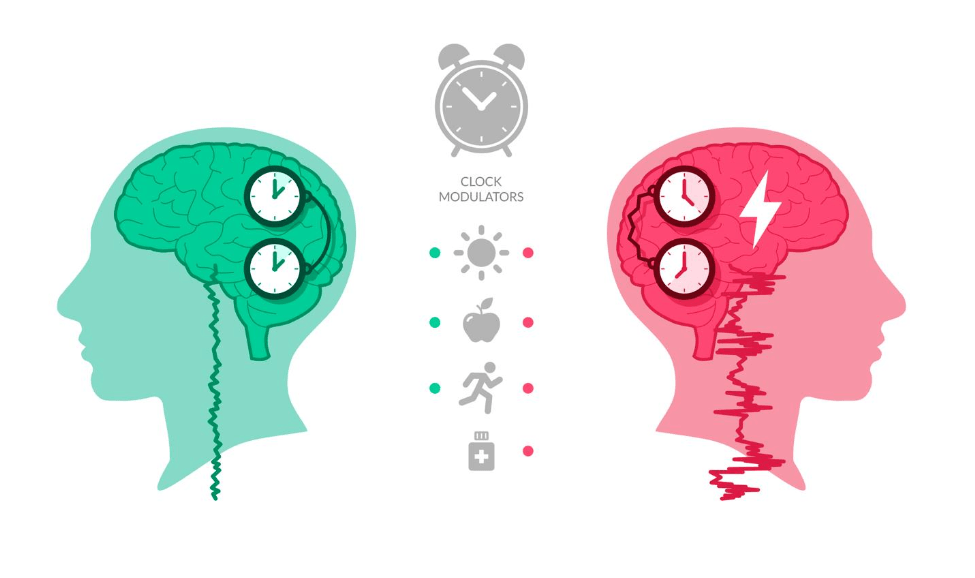
A variety of external cues could be introduced to the circadian clock to block or restrain seizures. High-throughput studies performed in vitro have uncovered many molecules capable of resetting the circadian clock. These molecules appear useful as “clock drugs,” to reset oscillators in epileptic patients. For example, rapamycin, a drug that inhibits the mTOR pathway, could reduce seizures as well as modulate the circadian clock in the brain. The external cues such as light, diet, and exercise, which act as clock modulators have also been shown to have antiepileptogenic effects. These findings support the investigation of other ways of resetting biological rhythms to improve seizure control and lessen cognitive and mood dysfunction in epilepsy. Appropriate clinical trials will be necessary to define the efficacy and safety profile of mTOR inhibitors and clock resetting approaches for treating mTLE, however.
Moreover, it will be interesting to examine whether interventions that improve cognition and mood at different phases would affect the circadian rhythm in the hippocampus and control seizures more effectively. Furthermore, the use of clock modulators may further improve the efficacy of neural progenitor cell transplants for controlling seizures in epilepsy, since clock genes have been shown to influence the proliferation and differentiation of neural progenitor cells. In this context, combined neural progenitor cell grafting into the chronically epileptic hippocampus and administration of circadian synchronizers, or phase-dependent grafting approach may improve graft cell survival and/or differentiation as well as neurogenesis in the host hippocampus.
Additive effects expected from such a plan may further diminish the frequency and intensity of spontaneous seizures and alleviate memory and mood impairments seen in chronic mTLE. Nonetheless, resetting the clock in epilepsy patients is not a straightforward approach, as the inter-individual variability in seizure occurrence can influence its efficacy. Clinical protocols for this intervention would, therefore, require a patient-specific approach upon tracking of seizure clusters during the day. Such measurements have immense value for developing patient-specific management of seizures using chronotherapy in the future.
These findings are described in the article entitled Chronobiology of limbic seizures: Potential mechanisms and prospects of chronotherapy for mesial temporal lobe epilepsy, recently published in the journal Neuroscience & Biobehavioral Reviews.
References:
- Leite Góes Gitai D, de Andrade TG, Dos Santos YDR, Attaluri S, Shetty AK (2019). Chronobiology of limbic seizures: Potential mechanisms and prospects of chronotherapy for mesial temporal lobe epilepsy. Neurosci Biobehav Rev, 98:122-134
- Akle V, Stankiewicz AJ, Kharchenko V, Yu L, Kharchenko PV, Zhdanova IV (2017). Circadian kinetics of cell cycle progression in adult neurogenic niches of a diurnal vertebrate. J Neurosci, 37: 1900-1909.
- Matos H, de C, Koike BDV, Pereira WDS, de Andrade TG, Castro OW, Duzzioni M, Kodali M, Leite JP, Shetty AK, Gitaí DLG. (2018). Rhythms of core clock genes and spontaneous locomotor activity in post- model of mesial temporal lobe epilepsy. Front Neurol.,, 9: 632.
- Hattiangady B, Shetty AK (2010). Decreased neuronal differentiation of newly generated cells underlies diminished neurogenesis in chronic temporal lobe epilepsy. Hippocampus, 20: 97-112.
- Waldau B, Hattiangady B, Kuruba R, Shetty AK (2010). Medial ganglionic eminence-derived neural stem cell grafts ease spontaneous seizures and restore GDNF expression in a rat model of chronic temporal lobe epilepsy. Stem Cells, 28: 1153-1164.
- Upadhya D, Hattiangady B, Castro OW, Shuai B, Kodali M, Attaluri S, Bates A, Dong Y, Zhang SC, Prockop DJ, Shetty AK (2019). Human induced pluripotent stem cell-derived MGE cell grafting after status epilepticus attenuates chronic epilepsy and comorbidities via synaptic integration. Proc Natl Acad Sci USA, 116: 287-296.









