
Photophobia describes an experience of discomfort or pain in response to light conditions. In normal conditions, it can be provoked using strong-intensity light. When it is provoked by light at normal intensity, it can be considered a symptom that is observed in many ophthalmological and neurological disorders. The most common conditions in which this alteration occurs are in patients with migraine and patients with ocular pathologies.
In migraine, photophobia is related to functional alterations of the trigeminal system, the thalamus, and the visual cortex. For these reasons, reducing the visual cortex pathological responsiveness to light may improve migraine patients. Non-invasive brain stimulation (NIBS) techniques use a physical agent like magnetic pulses, electrical fields, or ultrasound to modulate the cortical excitability and functions. We described a NIBS technique based on the application of strong static magnetic fields (tSMS) over the cortex. Thus, tSMS applied over the visual cortex can change brain activity and decrease the visual cortex excitability.
With the idea of using tSMS in migraine patients, we first studied its effect on experimental photophobia (visual discomfort experimentally induced in healthy subjects by an intense light). The static magnetic field was obtained by using a neodymium magnet. This is a type of rare-earth magnet; it is a permanent magnet made from an alloy of neodymium, iron, and boron with a tetragonal crystalline structure. This material is the strongest type of permanent magnet available in the market.
We performed a crossover, double-blind, sham-controlled study on twenty healthy volunteers. All subjects participated in two experimental sessions at least one week apart with different interventions (tSMS or sham) applied for 10 minutes over the occiput. In each session, subjects were seated in a comfortable armchair in a dark room, facing the wall, and received low-intensity and high-intensity visual stimuli before, during, and after the tSMS (real or sham) interventions. In this way, each session was divided into three blocks of 10 minutes and 16 visual stimuli each (8 low-intensity and 8 high-intensity). Visual stimulation was applied for 1 second every 39 seconds, and after each visual stimulation, subjects were asked to rate visual discomfort, using a visual analog scale (VAS), with 0 for no-discomfort and 10 for very-severe- discomfort. The figure shows a schematic drawing of the helmet with incorporating tSMS and the visual stimulation (LED) we used for our experiments.
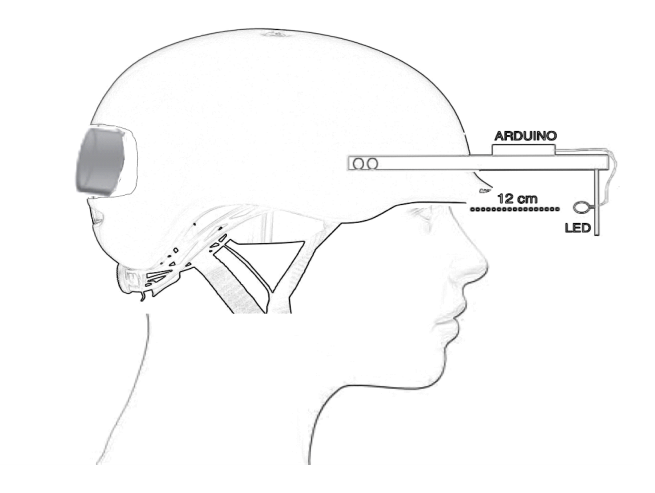
Credit: Vanesa Soto-Leon
We found that occipital tSMS reduces the visual discomfort evoked by high-intensity visual stimuli in healthy subjects. Specifically, the mean VAS was lower only for real tSMS compared to sham during the second half of the intervention block.
We conclude that focal static magnetic fields can interfere with responsiveness to high-intensity visual stimulation in healthy population. This result provides motivation for applying this novel NIBS technique, which is both portable and inexpensive, to move towards possible clinical application of tSMS in migraine.
These findings are described in the article entitled Transcranial static magnetic field stimulation (tSMS) of the visual cortex decreases experimental photophobia, recently published in the journal Cephalalgia.









