
Australia could be the first country in the world to completely eradicate cervical cancer, thanks to an extensive screening and vaccination endeavor. A new study published in the journal Lancet Public Health implies that by the year 2022 cervical cancer will be a “rare cancer” in Australia, with only about six cases per every 100,000 people.
Beyond that, the study suggests that within 20 years the disease could be effectively eliminated within the country. Death rates by cervical cancer are expected to decline to one in every 100,000 by 2034.
Cervical Cancer Rates In Australia And Around The Globe
Australia’s current rate of cervical cancer is about seven cases is every 100,000. This occurrence rate is already fairly low, about half the average of the world. Australia’s low cervical cancer occurrence rate has been attributed to national disease prevention projects, including an effective Human Papillomavirus vaccination project targeting girls created in 2007. This project was later expanded to target boys as well. The vaccination program augmented an already existing national cervical cancer screening program that was created in 1991.
Cervical cancer is the result of infection by one of the most prolific sexually transmitted diseases in the world, Human Papillomavirus (HPV). While cervical cancer can occur due to other causes, it is estimated that almost every case of cervical cancer, some 99.7% percent of cases are due to infection by HPV. HPV refers to a class of viruses that are spread by skin contact near the genitals during sexual intercourse. There are various types of HPV, some have a higher risk than other. It is possible to be infected with HPV and not suffer any ill effects, and indeed many women in the world will have HPV at some point in their lifetime yet display no symptoms. Cervical cancer is primarily the result of “high-risk” HPV infections.
Currently, cervical cancer is diagnosed in approximately 500,000 women every year around the world. The World Health Organization states that the disease is also responsible for the deaths of almost 250,000 women, mainly in middle-income and low-income countries.
Despite the prevalence of cervical cancer and HPV in many regions of the globe, health scientists say that cervical cancer is very easy to prevent, it just takes some concentrated effort. Researchers on the Cancer Council of New South Wales predicted the success rate of efforts to reduce cervical cancer rates. The researchers found that cervical cancer should be eliminated within the next couple decades if current efforts are sustained.
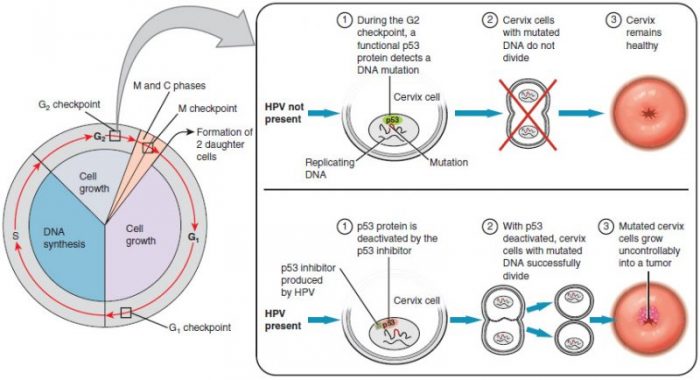
Though many cases of HPV heal on their own with no major damage, some “high-risk” cases will become cancerous, turning into cervical cancer. Photo: By OpenStax College – Anatomy & Physiology, Connexions Web site. https://openstax.org/books/anatomy-and-physiology/pages/1-introduction, Jun 19, 2013., CC BY 3.0, https://commons.wikimedia.org/w/index.php?curid=30148642
On Track To Eradication
The researchers modeled the trajectory of cancer occurrences based on vaccination data for HPV vaccines, data from cervical cancer screenings, and the natural history of the disease to estimate how frequent the disease would be per age group from the years 2015 to 2100. After analyzing the data, not only did the researchers find that the disease will be effectively eliminated by 2040, but that cervical cancer rates will decrease down to less than one in 100,000 for women if HPV screening continues to happen every five years and if people are given the vaccine.
The continued success of cervical cancer elimination projects will depend on the sustained implementation of vaccine and cancer screening programs. The path to implementing vaccination programs has been slow in some areas of the world, largely due to vaccine misinformation campaigns that attribute the scientifically unsupported development of autism or other forms of illness to vaccines.
Ian Frazer, a co-creator of the vaccine for cervical cancer, was excited about the news of Australia’s cervical cancer reduction and says the news made him “very proud that the research community can deliver the goods when it’s asked and can make a real difference in terms of world health.” Despite this, Frazer acknowledges there are still challenges on the horizon, particularly combating misplaced fears about vaccines spread by misinformation.
Screenings And Vaccinations
Frazer says that misinformation has made implementing vaccine programs more difficult, adding to the already existing logistical challenges of creating a nationwide vaccination program. As an example, Japan has seen vaccination rates for HPV drop to around zero, down from 70%. Meanwhile, the US has seen high HPV infection rates – around half of the US population between the ages of 18 to 59 is thought to be infected with genital HPV. Despite this, only about half of teenagers have received the HPV vaccine. Frazer says that reversing this trend and convincing people of the safety of vaccines “takes a lot of education to get there, it doesn’t happen overnight.”
In terms of screenings, cervical cancer screenings have proved tremendously effective at reducing rates of cancer within women. At least one study found that after Australia’s National Cervical Screening Program was created the number of women diagnosed with the disease dropped by over half its previous number. The country has continued to improve upon its screening methods since the screening program was created in 1991. Recently Australia transitioned from using a Pap cervical screening (a method of screening that looks for changes in the cervix) to a new HPV based test. The HPV based test only needs to be done every five years and it is capable of finding abnormalities within the cells, likely caused by HPV infections. The HPV test can predict abnormalities before they have surfaced, and the improved early detection of HPV is predicted to cut cervical cancer rates by an additional 20% and lower mortality.
Researchers from the International Agency for Research on Cancer have stated that the study is excellent of example of how “modeling can contribute to assessing national progress in cancer control.” They also state that high-quality data and reliable models are critical for health organizations and government bodies to effectively monitor health problems and plan intervention strategies for health problems in general. The researchers say that customizing intervention strategies for the needs of a geographical area will help lead to the global elimination of cervical cancer, not just in Australia.
Despite the challenges of implementing screening and vaccination programs in a region, some areas of the globe (other than Australia) are seeing improvements in cervical cancer prevention. Australia’s success with reducing the disease has provided a model for other countries to follow. Chief Director of the UK’s Cervical Cancer Trust, Robert Music, says the UK has adopted many of the techniques which have worked in Australia and that these techniques are beginning to pay off in the UK. Music says the research done by the cancer trust predicts elimination in vaccinated generations by 2040. Music explains:
“We must not lose sight of this goal and should strive to increase uptake of the preventative vaccination and screening programmes, especially among non-vaccinated women where incidence is set to rise.”










