Cancer is a very large and costly, in terms of lives and money, problem that the world faces. Recently, a new cancer “vaccine” is about to begin human trials after a very successful animal trial.
As we continued to study and understand treatment options for cancers, we have started to realize that there is a lot of potential in using our immune system to eradicate cancer. Treatment options like chemotherapy are effective in treating cancer, but they also diminish our immune system’s strength.
“Cancer affects all of us, whether you’re a daughter, mother, sister, friend, co-worker, doctor, or patient.” — Jennifer Aniston
Cancer cells are near impossible for our bodies to fight off normally because the cancer cells can be very similar to our healthy cells, which makes detecting them difficult. The cancer cells can also release certain chemicals to disguise themselves. These two aspects of cancer cells work to make sure that they remain undetected by our T-cells.
The basis of most immunotherapy research, like this one, is to find ways to bolster the power of the T-cells to detect and destroy cancer cells. Using mice, researchers from Standford University were able to to do just that.
The Mice Trials
Published two months ago, the researchers showed that by injecting mice with two immune-bolstering agents, they were able to greatly eradicate lymphoma in the mice and prevent it from coming back.
One of the agents was a short DNA component that boosted the expression of a specific receptor on the T cell and the other agent was an antibody that attaches to this receptor. This combination causes the T cell to go after the tumor.
The antibody is a component that is specific to the tumor. This means that once activated, the T cell will go after the tumors that have this and will not attack anything else. This minimizes the side effects of this treatment compared to something like CAR-T.
The researchers found that when presented with 90 mice that had lymphoma, 87 of them were cured of cancer completely. Three of them did develop cancer again, but an additional treatment of the agents eradicated it once more.
This represents an astounding success for treating cancers like lymphoma. However, this treatment option was not universal. Mice with breast cancer responded to the treatment, but not as effectively as those with lymphoma. Mice with colon cancer did not respond to the treatments at all.
This means that the agents used are not universal for all cancers, but the success means that if we find similar agents on other cancers we can develop similar treatments.
Phase 1 Human Trials
Now, Dr. Ronald Levy will be leading the phase 1 human trials along with other members of the mice study. They will be working with patients who have a particular subtype of lymphoma, low-grade B-cell Non-Hodgkin, using the agents and seeing if results will be similar to the mice trial.
Dr. Levy and his team are planning on two trials using 35 patients with the particular subtype of lymphoma. The patients will be subjected to a low dose of radiation and two rounds of the injections using the agents.
The agents being used in this human trial are produced separately by two other companies and have already been shown to be safe in humans. The treatment is considered a vaccine because it triggers the immune system to attack and destroy the tumors. Unlike a true vaccine, the treatment does not confer lifelong protection against cancer.
“Cancer didn’t bring me to my knees, it brought me to my feet.” — Michael Douglas
This trial will be used to test the dosage and safety of the agents in humans. Dr. Levy estimates that if approved by the FDA, the treatment will be available one to two years after.
Other Cancer Immunotherapy
There are other existing immunotherapies geared towards treating cancer. In 2017, the FDA approved a treatment known as CAR-T to treat certain types of leukemia and lymphoma.
In the CAR-T treatment, the immune cells of a patient are removed from their body. The cells are then genetically re-engineered to attack the specific types of leukemia and lymphoma. When these newly modified immune cells are placed back into the patient’s body, they go after the tumor cells.
Dr. Michelle Hermiston, who directs the pediatric immunotherapy program at UCSF (first place to implement the CAR-T treatment), is greatly interested in the work being done by Dr. Levy.
Dr. Hermiston told SFGate that the CAR-T treatment is being used only on patients that have failed traditional treatment options. It acts as a sort of last resort.
This is because the treatment is expensive and very labor-intensive. The side effects are also a bit distressing as they include organ failure, loss of B cell function, and confusion. However, it is a very effective treatment option for those that do not have other viable options as survival rates go from 10% to 60%.
“Having cancer does make you try to be better at everything you do and enjoy every moment. It changes you forever. But it can be a positive change.” — Jaclyn Smith
Dr. Hermiston hopes that if successful, the treatment by Dr. Levy can be used towards treating her patients with lymphoma.
Other immunotherapies include developing antibodies towards certain cancers so that they can be used to target these tumors and eliminate them. Alemtuzumab, an approved antibody, is used to target leukemia and lymphoma types that affect the immune system.
There are many other immunotherapies that have been approved or are in the works towards getting approved. As we have developed a better understanding of cancers and how to treat them, we are slowly growing our list of tools towards eliminating them from the population.
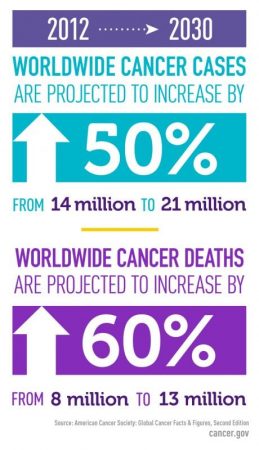
As cancer cases continue to rise, their burden on society will also increase. Developing effective treatment will work towards helping those affected as well as help improve society’s overall well being. Credit: Cancer.gov
According to the National Cancer Institute, over 1.5 million people developed some form of cancer in 2016 and over half a million died from a particular cancer. Beyond the terrible cost of human lives, the cost of cancer is expected to increase to $156 billion in 2020.
The burden that cancer places on society is great and will continue. Hopefully, treatments like these continue to be developed and we can find a viable cure for cancer.









