
Across a building or even a floor of the building, one encounters spaces with different thermal conditions. Through our everyday life, we move across these spaces with different degrees of warmth or cool multiple times.
Inherently, a sudden change in thermal conditions is likely to affect occupant thermal comfort. At the same time, there must be a magnitude of such temperature steps that would go unnoticed during our everyday life. Otherwise, we would be moving around in our homes or offices, reacting strongly to every minor variation in temperature.
Even though the difference in thermal environments and transitions across them are ubiquitous, thermal comfort standards and corresponding research have not focused a lot on understanding their effect on occupant comfort in actual work environments. The modern work environment is evolving fast, with trends like hot-desks, co-working spaces, work from home, and layouts that combine cellular and open-plan offices and workspaces and break rooms. Consequently, the design of modern office air conditioning must also be considerate of these changes.
To this end, a study was organized, across two workspaces — hospital wards for nurses and a typical office space — to gain a better perspective of how thermal transitions affect occupant satisfaction with and sensation of the indoor thermal conditions. Both studies used a mix of objective measurement of the indoor thermal condition and subjective feedback from the occupants. Occupant perspective of their thermal environment was gaged following their movement across different thermal zones. For the office space, this was between the cellular offices and the adjoining common spaces like pantry and hallways. The nurses have an active job, which meant they had frequent transitions between patient rooms, medicine room, reception, and the nurse’s break room. By covering the more active nurses and the near sedentary office workers, we were able to cover a reasonably wide range of activity range for indoor occupants.
During the study, participants indulged in their normal work behavior. The surveys were carried out while minimally inconveniencing them. Thermal sensation votes (TSV) were queried on a seven-point scale: “Cold” (-3), “Cool” (-2), “Slightly Cool” (-1), “Neutral” (0), “Slightly Warm” (1), “Warm” (2), and “Hot” (3). These surveys were of the so-called “right-now” type, i.e., participants were asked about their perception of the thermal environment at the moment and not their overall experience of their workspace.
The most interesting results of the study may be put into two categories. One was the stark contrast between the thermal comfort perception and needs of office workers and nurses. Due to the difference in activity levels, such contrast was expected in their steady state thermal perception sensation. But here, we saw it reflect in thermal comfort perception following spatial transitions as well.
Figure 1 gives the TSV and the corresponding temperature steps, for both workplaces. TSV for the two groups was quite distinct and differed even when preceded by a similar temperature step. The distinctions are stark enough that a computer program, without any other information than in Figure 1, was able to group votes into the correct workspace about 80% of the time.
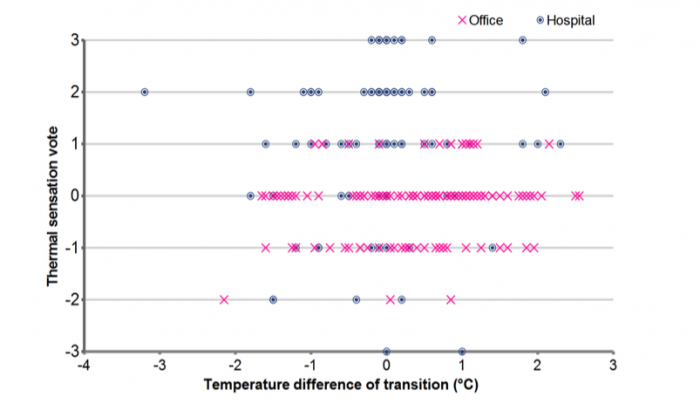
Figure 1: Scatter-plot of TSV and air temperature steps for hospital and office feedback together. Credit: Asit Mishra
The nursing staff found sensation slightly to the cool side of “Neutral” as most acceptable. For the office workers, it was slightly to the warmer side of “Neutral.” The difference between the two populations’ optimal points was about one unit on the seven-point TSV scale. Nurses’ thermal acceptability was also better following an experience of a 0.4 °C, or greater, temperature step. In the office, similar thermal step changes brought a feeling of warmth to the occupants. The 0.4 °C value came from instrument accuracy.
The explanation of this stark contrast is most likely the difference in the activity profile of the two populations. Unfortunately, this difference, as of yet, is not usually considered when designing hospitals. Often, patient thermal comfort criteria — which is closer to sedentary office workers — are extended to the entire ward, burdening the caregivers, who have different needs [1].
Figure 1 also contains the other interesting aspect: how do step-changes in indoor temperature, due to spatial transition, affect people? As may be noted from the plot, there is no discernible pattern to how TSV varies with the magnitude of the temperature step. From our observations, we can say that for steps of 2 °C or lower, TSV was not impacted significantly by the magnitude of the temperature step, neither for the active nurses nor the near sedentary office workers. As discussed earlier, the step changes might even have had small, positive effect on occupant thermal perception, this being more apparent for the nurses. This is in line with some earlier observations that noted that feelings of greater thermal comfort are more likely to come during transitions than under steady conditions [2].
This leads to the idea of thermal zoning of different portions of buildings. With set-points of different areas being maintained within ∼2 °C, the temperature steps are unlikely to cause inconvenience to occupants. They might even be welcome. Such zoning needs to take into consideration building orientation, usage, and occupant activity. When done appropriately, this can also lead to energy savings. Thermal zoning and variability within buildings may even help accommodate the greater integration of renewable energy in the grid by helping synchronize with the variable energy supplies.
These findings are described in the article entitled Occupant response to transitions across indoor thermal environments in two different workspaces, recently published in the journal Building and Environment. This work was conducted by M.G.L.C. Loomans, M.T.H. Derks, and J.J. Kraakman from the Eindhoven University of Technology, A.K. Mishra from the Eindhoven University of Technology and Berkeley Education Alliance for Research in Singapore, and H.S.M. Kort from the Eindhoven University of Technology and Utrecht University of Applied Sciences.
Acknowledgment:
The contributions and extensive cooperation from my co-investigators — Dr. Marcel Loomans, Prof. Helianthe Kort, Manon Derks, and Arjan Kraakman — is gratefully acknowledged.
References:









