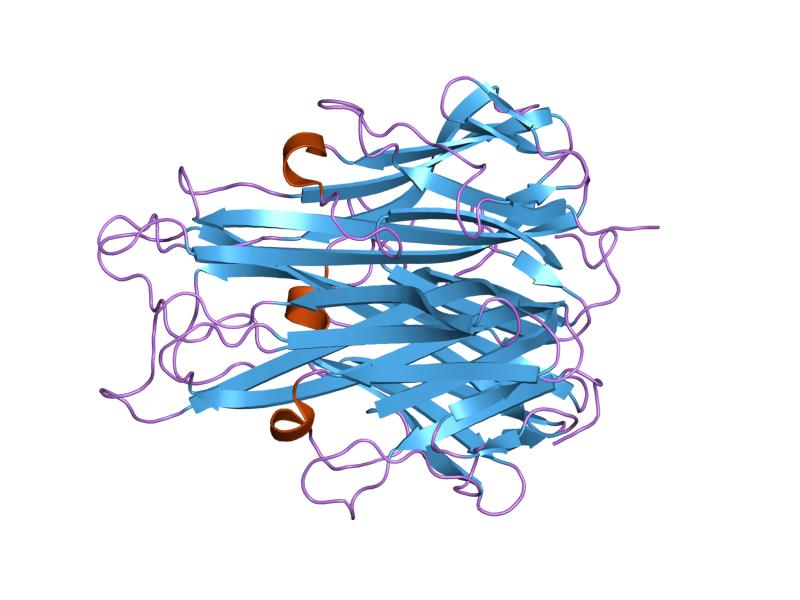
TNF is an important mediator that drives the pathogenesis of several inflammatory auto-immune diseases, including Crohn’s Disease and rheumatoid arthritis (RA). Treatment of these diseases has significantly improved since the introduction of therapeutic monoclonal antibodies that specifically target TNF (TNF inhibitors). Adalimumab is one of the five TNF inhibitors that is widely used in the clinic. To date, many studies focused on the drug, while surprisingly little is known about the target, TNF, during TNF inhibitor treatment.
Once in remission, a proportion of patients can successfully discontinue treatment, indicating that blocking TNF is no longer required for disease control. We, therefore, expected a decrease in TNF concentrations in patients who are in clinical remission. Following this, monitoring TNF during TNF inhibitor treatment could be a potential biomarker in predicting successful treatment discontinuation.
In order to investigate the relationship between TNF concentrations and the clinical response, we developed a new competition enzyme-linked immunosorbent assay (ELISA) which is able to quantify TNF in the presence of large amounts of adalimumab, i.e. a “drug-tolerant” assay. This assay was used to quantify TNF concentrations in 193 RA patients at baseline, before the start of adalimumab treatment, and during two years of follow-up. We demonstrated that circulating TNF concentrations were low at baseline but significantly increased upon adalimumab administration. Increased TNF concentrations upon treatment might seem counterintuitive since most patients do respond to TNF inhibitor treatment. However, this can be explained by a prolonged TNF half-life, due to binding of TNF to the TNF inhibitor, which themselves have a very long half-life of several weeks.
In contrast to what was expected, TNF concentrations did not go down over time in patients reaching remission. Instead, TNF concentrations remained extremely stable in the majority of patients for at least two years. A similar increase in TNF was found in healthy volunteers after one dose of adalimumab. Together, this implies that TNF in circulation during TNF inhibitor treatment is not primarily associated with disease activity and that TNF can, therefore, not be used as a biomarker to predict successful treatment discontinuation.
Although longitudinal TNF concentrations were extremely stable in the majority of patients, some patients had significantly lower TNF concentrations at week four. Remarkably, it appeared that, in particular, these patients with early low TNF concentrations started to produce substantial amounts of anti-drug antibodies (ADAs) over time. Previous studies demonstrated that the formation of ADAs is an important factor associated with non-response. This is supported by findings from our study, which demonstrates that patients with worse disease outcomes have early low TNF concentrations, associated with future ADA formation. Although further studies should elucidate the underlying mechanism (how is the drop in early TNF concentrations linked to a future appearance of ADAs, which associate with a non-response?), these results suggest a potential role for TNF measurements as a predictive biomarker for future ADA formation and for the identification of non-responders in the early phase of treatment.
Moreover, it is of major importance to understand the underlying mechanism of ADA formation. Why do some patients develop significant amounts of ADAs, while in others the formation of ADAs remains undetectable? Unraveling these mechanisms might help to optimize current TNF inhibitor therapies and possibly contribute to avoiding immunogenicity for future therapies.
This study also highlights a conundrum with respect to treatment discontinuation. We demonstrated that circulating TNF concentrations typically remain high, up to even half a year after adalimumab treatment discontinuation. So, circulating TNF is likely still blocked even half a year after adalimumab treatment discontinuation. The issue is: when did the treatment really stop? This is relevant when evaluating switch studies, studies aimed at evaluating the success of treatment discontinuation upon reaching remission. Usually, a washout period of the first TNF inhibitor (adalimumab) is taken into account. However, at the time treatment with a second TNF inhibitor starts, TNF may still be in complex with adalimumab. Therefore, evaluation of the treatment efficacy of the second TNF inhibitor might be influenced by the presence of TNF-adalimumab drug complexes that are still circulating. It also calls into question the effectiveness of temporal discontinuation of treatment in case of an infection or surgery.
Furthermore, data from this treatment discontinuation study suggests that an adalimumab concentration around as low as 0.1 μg/ml in circulation is sufficient for near-quantitative in vivo capture of TNF. In comparison, the therapeutic range for maximal clinical effect for adalimumab is 5 – 8 µg/ml. This implicates that a proportion of patients might not need to be exposed to drug concentrations in the range currently achieved by standard care and that serum drug concentrations could be reduced. This raises questions about the minimal amount of TNF inhibitor that is critical for maintaining a clinical response.
Therapeutic drug monitoring (TDM)-based treatment is an upcoming field and, in combination with clinical response, might help to identify the minimal amount of TNF inhibitor that is needed for maintaining clinical response. Consequently, the amount of administered drugs might be reduced.
These findings are described in the article entitled Dynamics of circulating TNF during adalimumab treatment using a drug-tolerant TNF assay, recently published in the journal Science Translational Medicine.
Citation:
- L.C. Berkhout, M.J. l’Ami, J. Ruwaard, M.H. Hart, P.O.-d. Heer, K. Bloem, M.T. Nurmohamed, R.F. van Vollenhoven, M. Boers, D.F. Alvarez, C.H. Smith, G.J. Wolbink, T. Rispens, Dynamics of circulating TNF during adalimumab treatment using a drug-tolerant TNF assay. Sci Transl. Med. 11, eaat3356 (2019).









