In Canada, approximately 3% of all traumatic injuries result in peripheral nerve damage resulting in many patients suffering from lifelong sensorimotor impairments. In severe cases, patients will undergo nerve repair surgery but this surgery is often delayed for months after the original injury. This means that at the time of surgery, the injury environment has many cells present that have lost their ability to promote nerve regeneration.
Understanding the mechanisms that enhance regeneration shortly after nerve damage will be essential in developing new therapies to more effectively restore functional recovery especially important for chronic injuries.
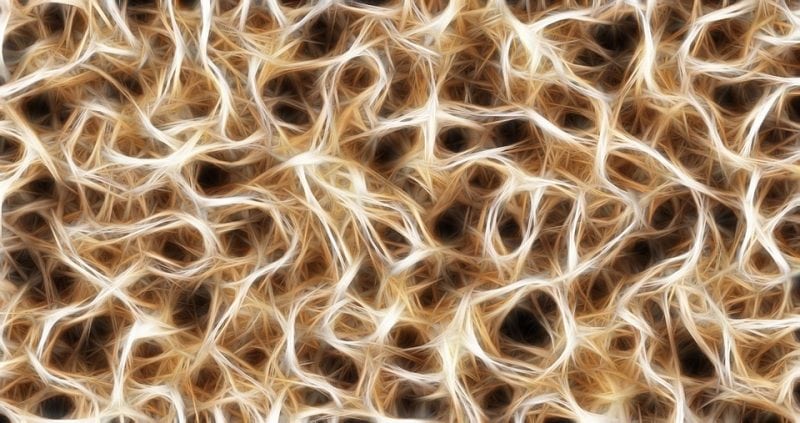
Decades of work have demonstrated the importance of Schwann cells as a support cell within nerves and as essential contributors to nerve regeneration. Yet, how these cells contribute to this process and what genetic factors underlie their regenerative abilities is not well understood. One tantalizing possibility is that Schwann cell behavior after injury is regulated by immune cells that are recruited to the injury site to aid in tissue repair. However, the role of immune cells, such as macrophages (comprising almost half of the cells within the acutely injured nerve), and their influence on Schwann cell function remains largely unexplored.
In our study, we sought to better understand this complex interaction and the specific macrophage-derived signals that might influence Schwann cell function. To this end, we first show that macrophages persist in the injured nerve in rodents and humans long after the initial stages of debris clearance. Second, we found that depletion of macrophages compromised Schwann cells regenerative capacity and led to long-term functional deficits, emphasizing the importance of macrophages to successful nerve regeneration. We then examined the gene expression profiles of macrophages within injured nerves to determine how they might communicate with Schwann cells. We identified many secreted factors including HBEGF, Gas6, IGF1, IFG2, FGF, IL6, VEGF and LIF, of which many of these are known to interact with Schwann cells. One gene of particular interest that was highly enriched in macrophages was Gas6.
Gas6 is a secreted ligand that binds the Tyro3 receptor known to be expressed by Schwann cells. Indeed, experiments in which we added or depleted Gas6 confirmed that macrophage-derived Gas6 acts to promote Schwann cell maturation, allowing them to form new myelin around regenerating axons, thereby enabling effective nerve regeneration. Further to this, we also identified a battery of additional neurochemicals that may positively influence Schwann cell function. Finally, we also demonstrated that in human nerve injury macrophages express Gas6. Together our study supports the notion that immune cells are essential players in nerve regeneration and demonstrate that macrophage-derived factors modulate Schwann cells to promote improved regeneration.
This work identifies unique therapeutic targets that could be used to maximize the regenerative processes and improve outcomes following nervous system injury. In the future, our laboratory aims to exploit these therapeutic targets to enhance nerve regeneration in chronic nerve injury. Ultimately, the knowledge we gain in rodent experiments will be applied to treat people who suffer from nerve injuries where current treatment approaches are inadequate.
These findings are described in the article entitled Macrophages Regulate Schwann Cell Maturation after Nerve Injury, recently published in the journal Cell Reports. This work was conducted by Jo Anne Stratton, Alexandra Holmes, Nicole L. Rosin, Sarthak Sinha, Mohit Vohra, Nicole E. Burma, Tuan Trang, Rajiv Midha, and Jeff Biernaskie from the University of Calgary.









