Degenerative brain diseases like Alzheimer’s disease are not only difficult to treat, they are difficult to detect. A team of scientists has recently developed a way of detecting early signs of Alzheimer’s disease, by using a simple blood test.
The study, which was recently published in the journal Nature, tests the blood for the presence of a substance called amyloid beta. Amyloid beta is a protein that is correlated with the development of Alzheimer ’s. The research was carried out by a group of scientists from Japan and Australia. The test was able to identify people who had amyloid beta in their brains with 90% accuracy during an experiment with around 370 subjects. The goal of the blood test was to predict the discovery of amyloid beta in a person’s brain because the protein builds up in the brains of those with Alzheimer’s disease.
A Blood Test For Proteins
Creating a successful test that could find levels of amyloid beta in the blood was difficult because very little of the protein is found in the bloodstream when compared to how much is found in the brain. Furthermore, previous studies struggled to find consistent correlations between levels of the protein in the blood and levels in the brain. The study was done on 121 people from Japan and 252 people from Australia. Both groups of test subjects included people with different levels of brain function, including those who had Alzheimer’s, some cognitive impairment, or normal cognition.
The normal methods of detecting amyloid beta in the brain were a brain scan or spinal tap. These procedures could find the plaque buildup caused by amyloid beta, but they are invasive and expensive. By contrast, the team of researchers from Australia and Japan devised a much less invasive procedure, enabling a blood test to be done for amyloid beta through the use of mass spectrometry.
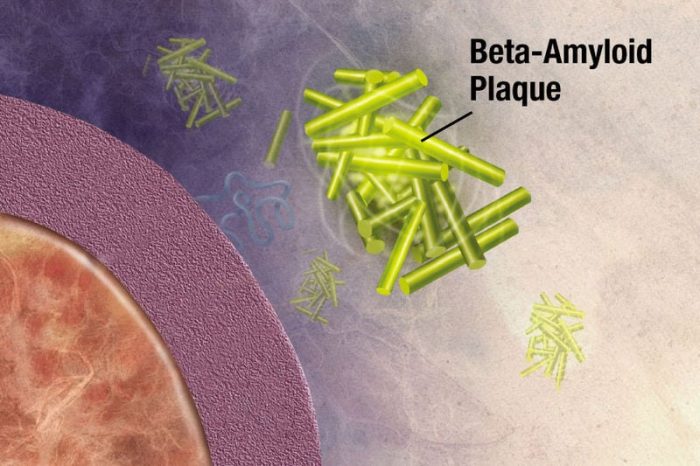
Photo: Beta-amyloid plaques in the brain interrupt the signals between synapses in those who have Alzheimer’s disease. Photo: National Institute of Health, Public Domain
Mass spectrometry is a technique which sorts the ions of a particle based on their mass-to-charge ratio, measuring the mass within a specific sample of an object. The use of mass spectrometry meant that much smaller amounts of amyloid beta could be detected in the blood. This means that instead of examining the total amount of a protein within the blood, the researchers instead calculated the relative ratios of amyloid beta within the blood. From these calculations, they were able to correctly discern, around 90% of the time, if amyloid beta was or wasn’t in the brains of their subjects. In the words of the researchers, the presence of amyloid beta in the blood is an “accurate surrogate” for the buildup of amyloid plaques within the brain.
The new study confirmed the findings of a smaller study done with blood tests last year. Randall Bateman, a researcher of Alzheimer’s at Washington University School of Medicine, was the lead author on the 2017 study and he is excited that the results confirmed his findings.
Says Bateman:
It’s a fantastic confirmation of the findings. What this tells us is that we can move forward with this [test] approach with fairly high confidence that this is going to pan out.
Implications For The Treatment Of Alzheimer’s
Alzheimer’s disease impacts around 5 million people within the United States, and around 520,000 people in the UK. Worldwide it is thought that around 44 million people have Alzheimer’s or a related form of dementia. The United States alone spends about $259 billion dollars a year fighting Alzheimer’s disease.
Scientists still aren’t sure of the exact cause of Alzheimer’s, but they do know that amyloid beta and another protein called tau play a role in its development. The buildup of tau and amyloid beta in the brain seems to start decades before the symptoms of Alzheimer’s begin to manifest, meaning that the new blood test could potentially spot an individual’s risk of developing Alzheimer’s 30 years before it happens. This would make the blood test an extremely useful early warning device and a powerful tool in the fight to find a cure for the disease.
Early detection of diseases is important because the earlier a disease is detected the sooner it can be treated and the more damage can be avoided. There is currently no treatment for Alzheimer’s disease, but the researchers are hoping that the test could create a list of potential candidates for clinical trials of treatments in the future. Having access to a cheap blood test could make it much easier for pharmaceutical companies to find subjects to test potential treatments on.
Furthermore, it is suspected that changes to one’s lifestyle can stave off the development of Alzheimer’s, so if an individual knows they are at risk they could make changes to lower the probability of developing it. It is thought that sleep habits, exercise, and diet could all play a role in the development of Alzheimer’s. Research into potential treatments for Alzheimer’s is continuing, and some recent findings provide cause for hope. When a treatment for Alzheimer’s disease is eventually discovered, early detection of the disease will be critical. The researchers emphasized the importance of learning to walk before learning to run, and that effective and reliable diagnosis of a disease is a necessary precursor to finding treatments for it.
The research team was careful to stress that although they are excited about the results, it is not currently practical for a clinical setting, as not everyone who the tests detect as having amyloid beta in their blood will actually have it. Furthermore, the presence of amyloid beta does not guarantee the development of Alzheimer’s.
Nonetheless, lead researcher Colin Masters hope there are clinical applications for their research sometime down the line. He hopes that eventually, people will be getting a checkup every five years after 55 to see if they are at risk of developing Alzheimer’s or not.
In the meantime and despite the success of the study, more work will have to be done to see if the tests continue to prove effective and viable for clinical applications. The researchers say they will have to see if the test proves effective when tested in larger, more diverse populations of test subjects.









