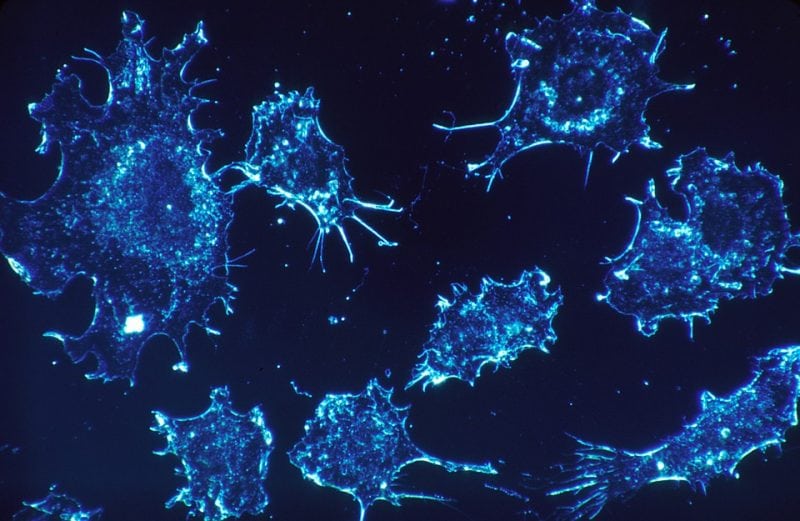
The liver is a popular destination for many spreading cancers, including colorectal carcinoma (CRC). This is not only owed to its anatomic location, but also likely due, at least partially, to its generally “tolerogenic” environment. Paradoxically, the liver is home to several cell types belonging to the innate arm of immunity. This is perhaps meant to allow for swift responses to invading bugs, including those accessing this vital organ through the portal venous system. However, the heavy presence of innate immunocytes, such as liver-resident macrophages (i.e., Kupffer cells), natural killer (NK) cells and mucosa-associated invariant T (MAIT) cells, could also influence the metastatic burden in cancer patients.
MAIT cells are unconventional, innate-like T lymphocytes with a unique invariant T cell receptor (iTCR) that is neither restricted by major histocompatibility complex (MHC) molecules nor responsive to peptide antigens. Instead, the iTCRs of MAIT cells recognize vitamin B metabolites of bacterial origin and certain drug compounds in the context of a monomorphic protein called MHC-related protein 1 (MR1).
MAIT cells also express a myriad of NK cell-associated receptors. Therefore, previous studies that have solely relied on staining for CD3 and NK cell markers to define conventional T and NK cells, respectively, may have easily overlooked MAIT cells. Thanks to the recent availability of tools that enable identification and enumeration of MAIT cells, we now know that these cells are a dominant population in the human liver, comprising up to 50% of all T cells. They can be relatively precisely immunophenotyped as CD3+Vα7.2+CD161++ and/or MR1 tetramer+ cells.
MAIT cells are inflammatory cells that exhibit a T helper 1 (TH1)- or TH17-type functional characteristics. They can express natural-killer group 2, member D (NKG2D), a receptor linked to anticancer and anti-pathogen immunity, as well as cytolytic effector molecules (e.g., perforin and granzymes) and interferon (IFN)-γ. Together, these attributes suggest a protective role for MAIT cells in anticancer immune surveillance. In contrast, the ability of MAIT cells to produce IL-17 may implicate them in tumor initiation and/or progression since IL-17 my promote neoangiogenesis and facilitate the recruitment of various suppressor cells into tumor microenvironments (TMEs).
Although a great deal has been learned about the antimicrobial properties of MAIT cells in recent years, a clear picture of MAIT cell roles, protective or pathogenic, in malignancies is still amiss. Several important studies have confirmed the presence of MAIT cells in primary kidney, brain, and colorectal cancers. However, whether the prominent localization of MAIT cells in the human liver would or could make a difference remains unclear.
To begin to address this question, we obtained and analyzed samples from patients with colorectal liver metastasis (CRLM). While several patients had received no chemotherapy prior to their liver resection surgery, a few had received preoperative treatment either with FOLFOX (a combination of folinic acid, 5-fluorouracil and oxaliplatin) or with FOLFOX plus the anti-angiogenic agent bevacizumab. For each patient, the frequencies of total and interferon (IFN)-γ-producing MAIT cells residing in the metastatic tumors, adjacent tissue (within 1-cm distance from tumors), and healthy tissue (at least 10 cm away from tumors) were determined.
We found that MAIT cells were readily detectable in the CRLM TME. To examine MAIT cells’ ability to mount pro-inflammatory responses, we exposed non-parenchymal mononuclear cells containing these cells to a panel of stimuli ex vivo. These included Klebsiella pneumoniae lysate (a crude source of MR1-restricted antigens), a potent bacterial superantigen called staphylococcal enterotoxin B, or a combination of interleukin (IL)-12 and IL-18, cytokines known to activate MAIT cells. While healthy liver-resident MAIT cells rigorously responded to all the above stimuli by producing IFN-γ, tumor-infiltrating MAIT cells were completely impaired, and tumor-margin MAIT cells were only partially active.
This was a consistent finding across the three sub-cohorts. In all patients, MAIT cells had apparently found their way into the tumor masses but were rendered dysfunctional within the tumors. Accordingly, we proposed that proximity to the TME, but not preoperative chemotherapy, was responsible for intratumoral MAIT cell impairments in CRLM patients. Our finding that healthy tissue MAIT cells from patients receiving systemic chemotherapy retained their IFN-γ production capacity lends additional support to the above notion.
MAIT cells express substantial levels of multi-drug resistance protein 1 (MDR1). Therefore, their apparent chemoresistance in our study was not surprising. This finding is important as it suggests that future treatment strategies to restore MAIT cell functions may be combined with select chemotherapeutics without much concern that the latter may harm MAIT cells.
Ongoing work in my laboratory is addressing MAIT cell roles in cancer in greater detail. We are also exploring whether and how MAIT cell manipulation may be of therapeutic value in the context of CRLM.
These findings are described in the article entitled Mucosa-associated invariant T cells infiltrate hepatic metastases in patients with colorectal carcinoma but are rendered dysfunctional within and adjacent to tumor microenvironment, recently published in the journal Cancer Immunology, Immunotherapy. This work was conducted by S. M. Mansour Haeryfar, Christopher R. Shaler, Mauro E. Tun-Abraham, Anton I. Skaro, Tina Mele, and Roberto Hernandez-Alejandro from Western University, Khashayarsha Khazaie from Mayo Clinic College of Medicine, and Alexandra J. Corbett from the University of Melbourne. The final publication is available at Springer via link.springer.com/…1007/s00262-017-2050-7.









