
This study is the first prospective, population-based prevalence study particularly designed for idiopathic normal pressure hydrocephalus (iNPH). The finding of a 3.7% prevalence among individuals aged 65 years and older confirms that iNPH is a fairly common condition. This prevalence is higher than in previous reports, probably because the disorder was screened for with questionnaires directed toward the general population.
Introduction:
Idiopathic normal pressure hydrocephalus (iNPH) is a progressive neurologic disorder affecting individuals over the age of 60, who, if left untreated, risk becoming wheelchair-bound and are more prone to dementia and incontinence. About seven out of ten see improvements after shunt surgery, but the outcome worsens with the progression of the disease, highlighting the importance of early diagnosis and treatment [1].
Even though the disorder was first described in 1965 [2], the prevalence in the general population is uncertain, and the knowledge regarding gender differences and age progression is limited. The prevalence of iNPH has been estimated to be between 0.5% and 2.9% among those aged 65 years and older [3-9]. However, previous studies have either been retrospective, based on selected materials, or designed for other conditions, like dementia. Further, varying definitions of iNPH have been used.
The objective of the present study was to estimate the prevalence of iNPH in a sample from the general population and to describe the differences in age and sex.
Methods:
During 2014, researchers randomly selected 1,000 individuals aged 65 years and older living in the county of Jämtland from the Swedish population register (SPAR) [13]. They received a questionnaire with seven questions, based on an American precursor [14], regarding typical iNPH symptoms, i.e. impairment of gait, memory, and bladder control. In total, 673 individuals (67.3%) completed the questionnaire.
Participants who reported two or more symptoms (n= 117), as well a randomized sample of individuals reporting less than two symptoms (n=51), were selected for further examination with a CT scan of the brain and clinical tests. To evaluate the iNPH symptoms, the following tests were used: The Hellström’s iNPH symptom scale, including a 10-meter walking test and grading of balance, gait, and urinary incontinence in ordinal scales [15-17]. In addition, the MMSE test, Timed up and go, and Rombergs’s tests were used [18-20].
The participants were diagnosed according to international guidelines, with the exception of the measurements of CSF opening pressure, which was not performed [10, 11].
Results:
The estimated overall prevalence of iNPH among individuals aged 65 years and older was 3.7 % according to the American European guidelines, and 1.5 % according to the Japanese guidelines, see Fig 1.
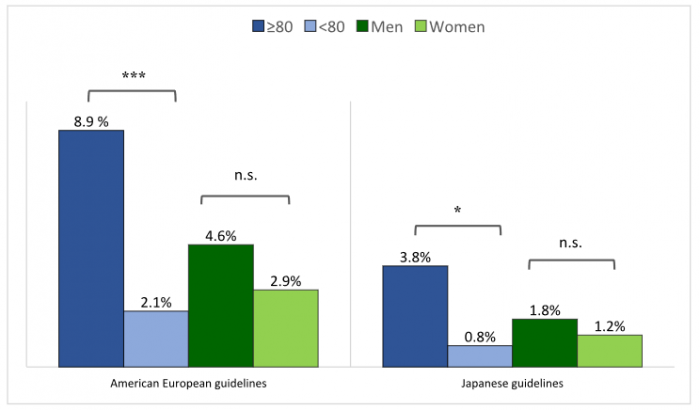
Fig 1. Prevalence of iNPH (possible iNPH excluded) in relation to age and sex with the American-European and Japanese guidelines, respectively. Figure republished with permission from PLOS One, from https://doi.org/10.1371/journal.pone.0217705.
The prevalence of iNPH was higher in the age group of those 80 years and above (8.9%), compared to those between 65 and 79 (2.1%), (p<0.001). No significant differences in the prevalence of iNPH were found between men (4.6%) and women (2.9%), (p=0.23).
Conclusions:
In this prospective, population-based study, the prevalence of iNPH was 3.7% among individuals aged 65 years and older. Thus, iNPH is a fairly common condition that should be increasingly recognized since it can be treated effectively by shunt surgery.









