
For a number of years, researchers have described endocrine (glandular) problems in some people with a history of concussion. These endocrine problems can emerge months or even years after the concussive injury and can involve a puzzling constellation of multiple hormonal problems.
It recently became apparent to scientists in the field that the underlying problem is under-performance of the pituitary gland. It is as if concussion in some people activates what amounts to a pituitary dimmer switch. This pituitary dimmer switch phenomenon is sometimes referred to as post-concussive hypopituitarism (PCHP).
The seriousness of PCHP lies in the central importance of the pituitary gland. In addition to secreting several vital hormones, including human growth hormone, this gland also controls key activities in the thyroid gland, adrenal glands, testes, and ovaries. For this reason, the pituitary is sometimes called the “master gland.”
In patients with PCHP, researchers have identified antibodies that attack the pituitary gland. These are sometimes accompanied by antibodies that attack the portion of the brain that controls the pituitary – the hypothalamus. It now seems plausible that PCHP is an autoimmune problem somehow activated by a concussion.
I became interested in the question of why some concussion victims develop PCHP and some do not. Another way of stating this would be: What are the risk factors for PCHP? I put forward what I hope is a plausible and useful working hypothesis to explain at least one risk factor (Hypoxic Stress: A Risk Factor for Post-Concussive Hypopituitarism? Medical Hypotheses, 2018; 121: 31-34.)
In short, my hypothetical mechanism involves the most important nutrient – oxygen. When the concentration of oxygen in the blood falls below normal levels – a condition called hypoxia – the body is at risk for elevated levels of inflammation. Inflammation, in turn, increases the risk of autoimmune activity. So, it is possible that such problems as asthma, emphysema, chronic bronchitis, obstructive sleep apnea, etc. are significant risk factors for PCHP.
A further layer of evidence for this hypothesis is that people with concussion history become more sensitive than other people to oxygen shortage in such situations as high altitude. This sensitivity can persist years after the concussion symptoms have apparently resolved. Since the post-concussive brain is hypersensitive to hypoxia in general, it is certainly plausible that the post-concussive brain is also vulnerable to autoimmunity triggered by hypoxia.
This still left an important gap in the hypothesis. Why doesn’t the entire post-concussive brain experience this hypoxic autoimmunity? Is there anything special about the pituitary-hypothalamic interface that makes it particularly vulnerable to this problem?
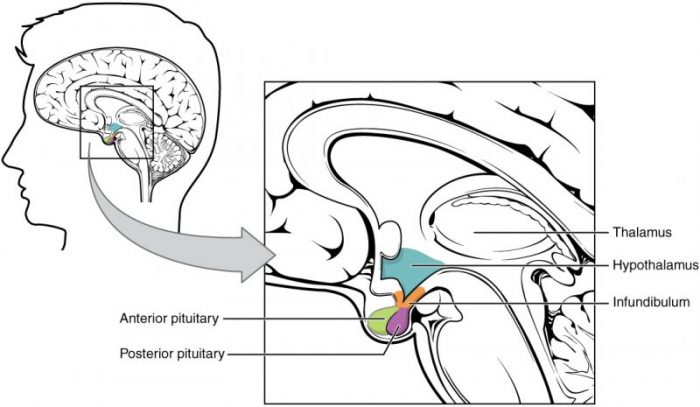
Source: Anatomy & Physiology, Connexions Web site. http://cnx.org/content/col11496/1.6/, Jun 19, 2013. Credit: OpenStax College via Wikipedia licensed under CC-BY 3.0
The answer may lie in basic anatomy. The hypothalamus contacts the pituitary through a slender stalk of brain tissue – the hypothalamic infundibulum. This stalk or infundibulum is only a few millimeters in diameter in the average adult human. The blood vessels in this delicate structure would seem to be particularly vulnerable during a concussive injury. In effect, the infundibulum may be a sort of choke point for hypothalamic-pituitary blood flow. The resulting disrupted blood flow could add local hypoxia to any systemic hypoxia.
In summary, I hypothesize that hypoxic stress from various systemic causes and local hypoxia at the infundibular choke point aggravate each other. This results in elevated levels of inflammation at the brain-pituitary interface, which in turn activates the autoimmune pituitary “dimmer switch.”
If this hypothesis is supported by future studies, concussion victims could be protected against long-term endocrine problems by early initiation of various types of respiratory therapy and exercise. This may include conventional medical interventions, lifestyle changes (smoking cessation, aerobic exercise, etc.), and non-Western techniques such as yoga. As a doctor of chiropractic, I am especially interested in the potential of chiropractic adjustments to prevent PCHP by improving respiratory function as well as local and systemic circulation.
These findings are described in the article entitled Hypoxic stress: A risk factor for post-concussive hypopituitarism? recently published in the journal Medical Hypotheses. This work was conducted by Charles S. Masarsky from Vienna Chiropractic Associates, P.C.









