
Cystinosis is a genetic disease that leads to the accumulation of cystine and the formation of intracellular crystals throughout the body, including in the kidney and cornea.
The crystals form inside lysosomes because of the loss of cystine efflux transporters that result in accumulation above the solubility limit, leading to crystallization. The crystals in the kidney are hexagonal, while those in the cornea are needle-shaped and likely extracellular. The cystine crystals in the cornea are predominantly located in the stroma, which is the thickest layer of the cornea and is rich is keratocytes and collagen.
We hypothesized that the needle-shaped crystals form in the stroma due to the presence of collagen. To test our hypothesis, we first explored crystallization of cystine in vitro in the presence of collagen and other polyelectrolytes. We observed that cystine precipitated into hexagonal crystals in buffers and in the presence of certain polymers, such as polyethylene glycol (PEG) and polyvinylpyrrolidone (PVP). However, in the presence of carboxymethylcellulose (CMC), which is an anionic polyelectrolyte, the crystals assumed a smaller and more spherical shape, and in collagen, which is also anionic in nature, the precipitates were long and cylindrical-shaped, which is similar to those formed in the cornea. These results supported the hypothesis and also suggested that the charge-charge interaction between the cystine and the polyelectrolyte plays a role in crystallization.
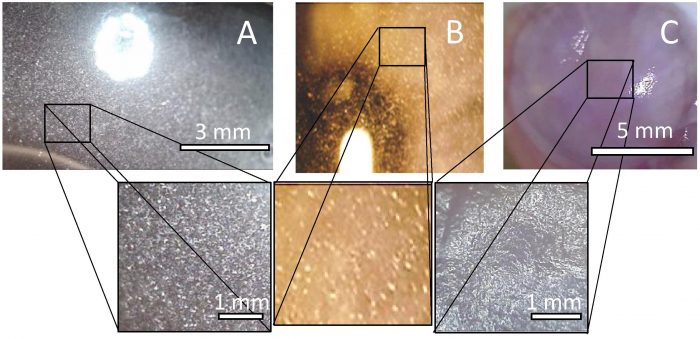
Fig. 2. Representative image of cornea with (A) cystine crystals via cysteine (5%) loading and oxidation; (B) Cystinosis patient (Liang et al., 2015), Copyright IOVS Journals © 2011. Printed with permission; and (C) cystine crystals via saturated cystine diffusion.
To further test the hypothesis, an ex vivo model was designed to determine the crystal shapes that will form in the stroma. Cadaver rabbit eyes were supersaturated with cystine to drive crystal formation. It was observed that the shape of the crystals depended on the degree of super-saturation, and under a low degree of super-saturation, the crystals were needle-like and the overall appearance of the crystal-loaded eyes was very similar to that of a Cystinosis patient.
The results indicate that in addition to the normal intracellular accumulation, the cornea has an additional mechanism that leads to the formation of needle-like extracellular crystals. The mechanism likely begins with the formation of the intracellular crystals in the keratocytes, just as in the other parts of the body. Eventually, the keratocytes undergo apoptosis during the natural healing response which releases the cystine crystals into the stroma. Once released, the crystals interact with the stromal collagen and further adsorption of dissolved cystine on to the collagen surface and heterogeneous nucleation and the needle-like crystals. This hypothesis assumes that in presence of collagen, the needle-like structures are more stable than the hexagonal crystals found in other parts of the body, so that, over time, the crystals from the ruptured cells dissolve to form the needle-like crystals.
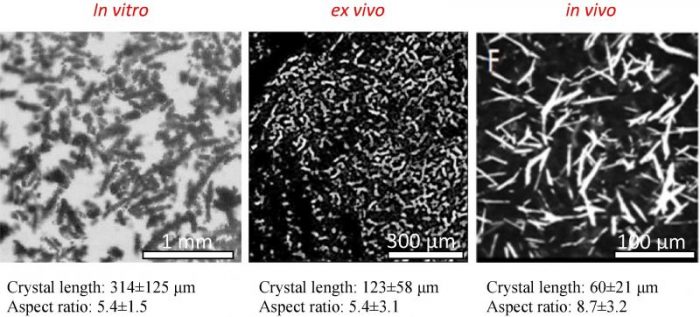
Fig. 3. (Left) Representative microscope image of cystine crystals created by cystine precipitation in presence of collagen; (Center) Representative microscope image of cornea loaded in saturated cystine solution for 10 days; (Right) confocal microscopy evaluation of anterior stroma corneal layers of cystinosis patient (Liang et al., 2015). Copyright IOVS Journals © 2011. Printed with permission.
The study does not provide conclusive evidence; however, the proposed hypothesis does explain the discrepancies between crystal shape in the cornea and the rest of the body. The stromal collagen plays an important role in crystal formation which was demonstrated by the in vitro ex vivo models. Additionally, the ex vivo model can be used as a testbed for future studies for understanding and treating cystinosis.
These findings are described in the article entitled Potential role of stromal collagen in cystine crystallization in cystinosis patients, recently published in the International Journal of Pharmaceutics. This work was conducted by Phillip Dixon, Keith Christopher, and Anuj Chauhan from the University of Florida.









