Chronic liver disease (CLD) is a leading cause of death for all Americans. Notably, it is the fourth leading cause of death in those 45-54 years of age and the sixth leading cause of death among Hispanic Americans. Traditionally, the leading contributors to CLD in the US were infection with hepatitis C and alcohol consumption2.
Data from a variety of national databases have provided a valuable perspective on the landscape of CLD and show the fatal impact of CLD on the US population. Importantly, these data show that the prevalence of CLD is on the rise despite major medical breakthroughs over the past decade, such as curative treatment for hepatitis C. This continued rise in the burden of liver disease is attributed largely to both increasing rates of non-alcoholic (fatty) and alcoholic liver disease3.
Given the changing landscape of liver disease, epidemiological studies will play a key role in deterring the ominous trend seen for liver disease-related outcomes. In other states battling specific diseases, geographic variations have led to impactful preventive measures. For example, description of the “Stroke Belt” in Southern states led to better understanding of demographic and healthcare system determinants of health with the establishment of research and clinical collaboratives aimed at reducing health disparities4, 5. Similarly, in an analysis of geographic variations, heart-healthy policies and built environment characteristics significantly impacted cardiovascular mortality6. Geographic variations in the burden of liver disease have not been explored in detail but may be an important step in influencing a field that is currently changing.
A recent study aimed to look at the inter-state geographic variability in liver disease mortality while assessing important co-morbid conditions in an effort to inform future public policy, guide research, and resource allocation. This study, published in the American Journal of Medicine, was a cross-sectional analysis of state-specific liver disease mortality rates and factors to be associated with liver disease mortality at a population level. Data was gathered from the Centers for Disease Control (CDC) and the 2010 Census and analyzed to describe and understand the relationship between liver disease mortality and geographic location. Factors that can influence this relationship such as viral hepatitis, alcohol consumption, and obesity rates as well as race, ethnicity, and household income were also analyzed.
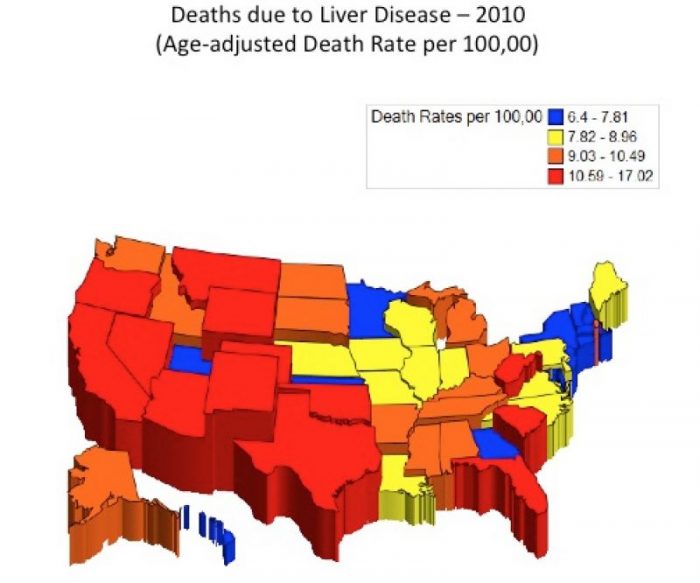
Republished with permission from the American Journal of Medicine from https://doi.org/10.1016/j.amjmed.2018.01.047.
The authors show significant variability in liver-disease related mortality ranging anywhere from 6.4 to 17.0 per 100,000 (Figure 1) with states in the west and central southwest carrying some of the highest liver disease mortality rates. Furthermore, while alcohol consumption and obesity significant risk factors liver disease, the study showed that these factors do not explain the geographic variability of liver disease mortality noted in the study. However, race and ethnicity impact liver mortality, with a strong correlation seen between states with higher rates of Hispanic individuals having higher rates of liver disease-related death. The study also found a statistically significant association between liver disease mortality and median household income.
The results of this study are significant as they can be used to identify modifiable drivers of liver disease-related mortality. Based on this study, future work aimed to understand the geographic variations in liver disease-related mortality will be revealing. For example, assessing variation in state and national public funding to study chronic liver disease care, variation in alcohol-related public policy, as well as public health resources to manage substance use disorders and availability of specialists and transplant centers need to be explored further.
Finally, investigation of other socioeconomic variables such as access to health insurance, income inequality, and build environment resources will be meaningful in understanding the variations in liver disease mortality seen. Together, this line of inquiry can target the efforts needed to curtail the growing epidemic of liver disease from funneling resources for research focused at dissecting disease mechanisms, testing treatments, and implementing preventive strategies where they are needed most.
These findings are described in the article entitled Geographic Variability in Liver Disease-Related Mortality Rates in the United States, recently published in the American Journal of Medicine. This work was conducted by Archita P. Desai from the Liver Research Institute, Prashanthinie Mohan and Anne M. Roubal from the University of Arizona, Ricki Bettencourt from the Department of Family and Preventive Medicine, and Rohit Loomba from the University of California at San Diego.
References:
- Heron M. Leading Causes for 2010. National Vital Statistics Reports. 2013;62(6):1-96.
- Carrion A, Ghanta R, Carrasquillo O, Martin P. Chronic Liver Disease in the Hispanic Population of the United States. Clin Gastroenterol Hepatol. 2011;9(10):834–e110.
- Kim, D. et al. Changing Trends in Etiology- and Ethnicity-Based Annual Mortality Rates of Cirrhosis and Hepatocellular Carcinoma in the United States. Hepatology. 2018. doi:10.1002/hep.30161
- U.S. Census Bureau, 2006-2010 American Community Survey. Table S1901. Income in the past 12 months (in 2010 inflation-adjusted dollars). Retrieved from https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t. Accessed August 17, 2016.
- Udompap P, Kim D, Kim R. Current and Future Burden of Chronic Nonmalignant Liver Disease. Clinical Gastroenterology and Hepatology. 2015;13(12):2031–2041.
- Xu J, Murphy S, Kochanek K, Bastian B. Deaths: Final Data for 2013. https://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_02.pdf. National Vital Statistics Reports Vol 64 No. 2. Hyattsville, MD: National Center for Health Statistics. Published Feb 2016. Accessed August 17, 2016.









