
When I first started working with upper motor neurons, I did not realize that the path would have such high levels of friction and be filled with so many hurdles.
First of all, many in the field did not appreciate the importance of upper motor neurons. They were very few in numbers, hard to visualize, observe and study. All neurons in the brain looked alike and the brain was so complex and heterogeneous. It did not make sense that I would want to study a very small neuron population that makes less than 0.001% of all neurons in the brain. “It is just a waste of time” I was told many times. Plus, there were no tools, no model systems, no reagents, nothing to detect them and to set them apart from other cells and neurons in the cerebral cortex. I was one young international women scientist with a name nobody can pronounce, and yet I was on a mission.
I think being an incurable optimist and a stubborn person helped me keep my head up and pay attention only to things that mattered. I knew the upper motor neurons were important, I knew they act as the “spokesperson” of the cerebral cortex when it comes to initiation and modulation of voluntary movement. I knew that every movement that we make which required cognitive input such as opening the door with a key, dancing, walking, playing music instruments, using sign language, all required the orchestrated activity of the upper motor neurons, which collected information from many different regions of the brain, integrated them into one signal and conveyed that signal to spinal cord targets to initiate movement. They work with such high speed and precision that we do not even realize we use them so often and that we depend on them to be ourselves and to be human. Their degeneration is characteristic of many neurodegenerative diseases, especially the ones that affect movement and motor function. When upper motor neurons begin to die, patients lose their ability to move their arms, legs, fingers, hands, and gradually they become trapped in their own bodies with a clear cognition and memory function, but no movement.
Because upper motor neurons act as the spokesperson, I wanted to be their spokesperson as well, and tried to tell everyone how important they are, and that we need to develop ways to improve their health with respect to disease. Many people said “neyyy, they are last to degenerate and their death is an outcome of spinal motor neuron loss, so they can never be a feasible target for any treatment. We need to focus on the spinal motor neurons”.. Aghh..
This was the dogma covered in medical school books, published in the 1960s, 70s, and all the faculty who graduated at those times believed it to be true: “Who cares about the upper motor neurons?” they asked, with a sign of humiliation, because they learned that degeneration is unidirectional, moving from periphery to the brain and brain neurons were the last resort and therefore upper motor neuron degeneration was just a mere consequence of ongoing degeneration. They did not contribute anything to the disease pathology; their death was just a byproduct. Les Turner ALS Foundation believed in me and supported me and I did not give up even six of my RO1 applications were consecutively triaged without even being discussed. Comments were very similar: “this reviewer is not convinced that studying the biology of upper motor neurons would contribute to the understanding of overall disease pathology, therefore significance was deemed low”.
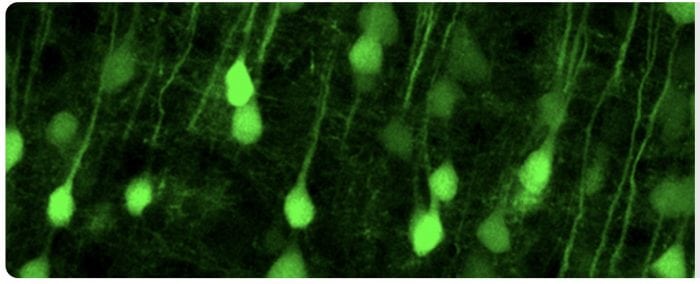
Upper motor neurons made fluorescent in the Ozdinler Lab. Credit: P. Hande Ozdinler
Well, just because we do not see, does not mean it does not exist and just because these people did not appreciate their importance, upper motor neurons did not lose anything from their importance. I continued working at least 12 hours a day and minimum 6 days a week.
We made the first reporter line for the upper motor neurons, UCHL1-eGFP mice. In these mouse models, the upper motor neurons were genetically labeled with eGFP expression, which was stable and long-lasting, allowing us to see and study the upper motor neurons with such cellular precision that was not possible before.
We realized something odd. The apical dendrites, the long extension that projects to the top layers of the brain where upper motor neurons collect information, were disintegrating in disease models; they were filled with vacuoles and falling apart even at the very early stages of the disease, even when no symptoms are observed. We observed the same cellular pathology in many different disease models, suggesting that upper motor neuron degeneration was indeed a very early event in the disease and that perturbations in the health and integrity of these neurons precede overwhelming disease pathology.
Ohh my.. This was just the opposite of what they were taught back in the day. So, of course, they said that I study mouse phenomena and this has no relevance to human and that human pathology would, of course, be as they suggest.
I was also curious. Could this be just a phenomenon observed in the upper motor neurons of mice or would the same cellular pathology occur in the human? I was lucky because Dr. Eileen Bigio thought this question was important enough to utilize the very precious post-mortem human samples donated by patients with ALS, ALS/FTD and control population. After careful investigation, we realized something remarkable! The apical dendrites of almost all upper motor neurons in ALS patients with a broad spectrum were disintegrated, filled with vacuoles, fragmented, and falling apart. The cellular pathology was so intense that it was almost obvious that this has been an ongoing cellular degeneration that just cannot happen overnight. Yes, what we discovered in the mouse was also true in the human! This was a remarkable finding because we realized one more time that focusing our attention to the neurons and studying neurons at a cellular level will be translational. Understanding why upper motor neurons die at a cellular, genetic and molecular level will reveal the underlying cellular pathologies that occur in humans. We were on the right path and we already generated the tools, the model systems, and laid the foundation for the path to follow.
So now people began to pronounce my name correctly, and I found myself on the invitation list for some international conferences. People then began to say: “We all knew upper motor neurons were important”.. I got my NIH RO1 and NIH R21 and foundation grants. Upper motor neurons started to climb to the center stage, where they belonged.
We even moved one step further and started to claim that by improving the health of the upper motor neurons, we can improve the health of the spinal motor neurons and even the neuromuscular junction. Right at that time, Dr. Svendson’s group published a paper showing exactly what we have been postulation. So we were not alone anymore. Dr. Vucic and many others also started to publish revealing how a cortical dysfunction is an early event in ALS and other motor neuron diseases and how the cortex contributes to disease pathology.
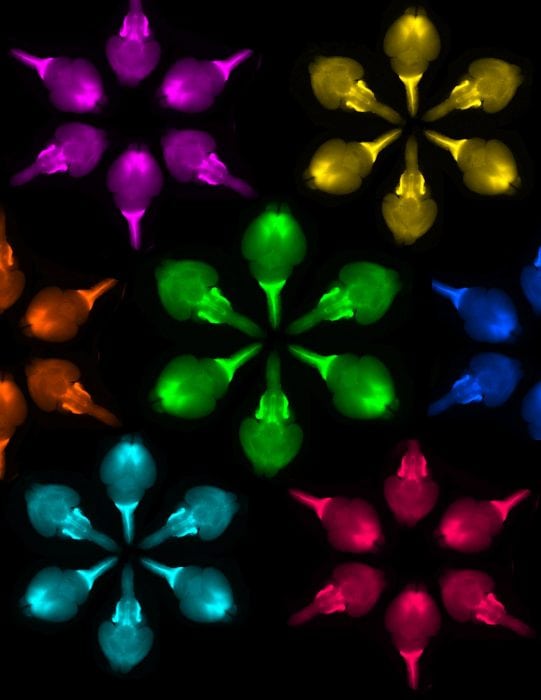
OzdinART generated by Dr. Ozdinler using transgenic mouse brain images. Credit: P. Hande Ozdinler
It was time to develop a drug discovery platform using upper motor neurons. Their improved health would be read out to determine if the compound of interest would be a good candidate or not. What a crazy idea, right? If you think about it, there have been more than 34 clinical trials that failed and none of them ever considered the health of upper motor neurons as a preclinical assessment. And yet, the spell could be in the upper motor neurons, because they are the ones that modulate the activity and function of the spinal motor neurons and they are the ones that collect, integrate and transmit cortical input to spinal cord targets. So we worked and worked and worked to generate the first platform that uses many different diseased upper motor neurons as a readout for preclinical assessment. Dr. Richard Silverman supported our platform and we received NeuroNXT grant to develop it further. Our goal is to increase the success rate of future clinical trials and to help drug companies to make educated guesses on which subset of the patient population to include in their studies. I am sure we will succeed. The patients are waiting, and we do not have the luxury to fail again and again and again.
Maybe because I spent so much time with these neuron populations, I formed a strong bond with them. It would not be a lie, if I told you that they started talking to me, revealing their cellular secrets. We now begin to understand why the upper motor neurons become vulnerable early in the disease, which genes they choose to express to protect themselves, and how they declare apoptosis, upon the realization that damage is beyond control. They reveal their secrets to us and it is impossible not to respect them, their fight to stay alive and their dignity as they try to keep working even to the last drop of their energy. I think after all that we have gone through, upper motor neurons began to like me as well. I feel very lucky.
One early morning I got an e-mail from NOBEL Forum asking me to attend the 2016 symposium at Stockholm. I thought somebody was pulling my leg and I even wrote back asking if they were sincere in their invitation. They replied back with a list of reasons why I was invited and I was flabbergasted. They said our lab was the first to label these neuron populations, first to develop AAV-mediated gene delivery approaches, first to characterize the underlying cellular causes of their vulnerability, first to generate and characterize novel model systems with upper motor neuron degeneration,.. and oh my somebody was reading our papers! 100 people were invited worldwide and I was one of them. I was not only invited to attend but also was given a platform to give a talk about the importance of upper motor neurons. Going from “excuse me what was your name and who cares about upper motor neurons” to “you are cordially invited to NOBEL Forum” was a sharp turn. What a day it was.. After my seminar, my 14-year-old son told me: “Mom, I think you are onto something”.
Yes, I was and I am onto something: making the world a better place by focusing on the biology and pathology of upper motor neurons, the neurons that help us enjoy being alive by allowing us to laugh, dance, walk, talk, and be as human as possible! I am onto helping them regain their health so that ALS patients, and other patients who become diseased because their upper motor neurons lose their health and integrity, can be happy again!
We still have not touched the finish line, but the path is clear and we have more determination than ever. I also received my tenure at Northwestern, people now call me Dr. Ozdinler, and when my grants are reviewed I at least get very high scores on the Significance section!

OzdinART generated by Dr. Ozdinler using motor cortex and astrocyte tissue culture image. Credit: P. Hande Ozdinler
As I write this text, my upper motor neurons are working, and I am thankful to them. And, if you laughed at any point, your upper motor neurons worked as well.
These findings are, in part, described in the article entitled Incorporating upper motor neuron health in ALS drug discovery, recently published in the journal Drug Discovery Today. This work was conducted by InaDervishi and P. Hande Ozdinler from Northwestern University.
All OzdinART images are used to generate funds to support innovative and collaborative research originated by early stage investigators by the Art Loves Science Foundation (www.artlovesscience.org ). If you would like to support, please write to [email protected].
References
- Yasvoina MV, Genc B, Jara JH, et al. eGFP expression under UCHL1 promoter genetically labels corticospinal motor neurons and a subpopulation of degeneration-resistant spinal motor neurons in an ALS mouse model. The Journal of neuroscience: the official journal of the Society for Neuroscience 2013;33:7890-7904.
- Jara JH, Villa SR, Khan NA, Bohn MC, Ozdinler PH. AAV2 mediated retrograde transduction of corticospinal motor neurons reveals initial and selective apical dendrite degeneration in ALS. Neurobiology of disease 2012;47:174-183.
- Genc B, Jara JH, Lagrimas AK, et al. Apical dendrite degeneration, a novel cellular pathology for Betz cells in ALS. Scientific reports 2017;7:41765.
- Genc B, Ozdinler PH. Moving forward in clinical trials for ALS: motor neurons lead the way please. Drug discovery today 2014;19:441-449.
- Dervishi I, Ozdinler PH. Incorporating upper motor neuron health in ALS drug discovery. Drug discovery today 2018.









