
The eye is one of the most important and complex organs in our body. A variety of causes, including injuries or diseases such as diabetes, glaucoma, macular degeneration, uveitis, cataracts, blocked blood vessels, complications of eye surgery, and inflammation of optic nerve may cause partial vision loss or blindness.
In order to understand the pathogenesis of ocular diseases, various components that operate within the eye were studied. Dysregulation of some ocular constituents provided beneficial pharmacological manipulation. We found that retinal extracts from man, guinea pig, hog, and rabbit eyes contain an angiotensin-converting enzyme (ACE). This enzyme was far more active in the retina and retinal microcapillaries than in plasma. ACE is included in two proteolytic axes, renin-angiotensin and kallikrein-kinin systems (Fig. 1).
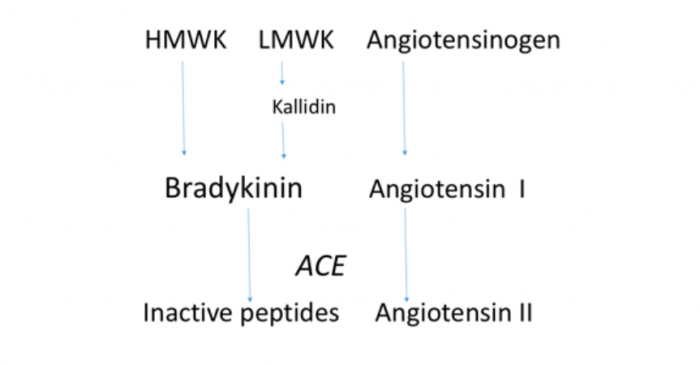
Figure 1. The peptides in the KKS and in the truncated portion of the RAS.
The RAS components involve almost twenty angiotensin peptides and more than twenty enzymes (peptidases), and six known receptors. Angiotensin II is a potent vasoconstrictor and stimulant of the synthesis of aldosterone; it participates in regulation of blood pressure, fluid volume, electrolyte balance, and inflammation. Its actions are regulated through the activation of two types of angiotensin II receptoprs, AT1 and AT2. Kallikreins release potent vasoactive peptides, kinins, from endogenous substances called kininogens. There are two types of enzymes called kallikreins, plasma and tissue kallikrein. Plasma kallikrein releases bradykinin (nonapeptide) from high molecular weight kininogen (HMWK), while tissue kallikrein releases kallidin (lys-bradykinin) from low molecular weight kininogen (LMWK). Kallidin is subsequently enzymatically converted to bradykinin. Bradykinin acts mainly through bradykinin 2 (B2) receptors in multiple tissues increasing vasodilation, vascular permeability, sweating, and increases intracellular calcium in smooth muscle cells. Angiotensin converting enzyme (ACE) inactivates bradykinin and activates angiotensin (it converts angiotensin I, inactive decapeptide, to biologically very active octapeptide, angiotensin II). KKS frequently counterbalance the RAS, but in some situations they act in the same direction, as during tissue injury. Their relationship needs further investigations in order to get detailed knowledge which may aid in developing drugs that act on both systems. Credit: Rajko Igić
I came from Sarajevo to Dallas, Texas, during my summer holiday, where, at the Southwestern Medical School, continued to do the kind of research I could not possibly accomplish in Yugoslavia. In Dallas, there was much better equipment to measure enzyme activity than in my laboratories in Sarajevo or Tuzla, where I became a chairman of the Department of Pharmacology at the medical school.
Working in Dallas made it possible for me to study ACE in human tissues since there were many accidents and murders, and untaken bodies autopsied at the department of forensic medicine department could be used for scientific studies. Thus, I continued my studies of ACE and renin in the retina that I began in Sarajevo. In 1977, I reported our findings at the Houston Conference entitled “Central actions of Angiotensin and Related Hormones,” and in the Liječnički Vjesnik, a medical journal published in Yugoslavia.
In 1996, van Haeringen noticed in the British Journal of Ophthalmology: “Ophthalmic literature concerning the RAS started in 1977 with a study by Igić and coworkers on the detection of ACE activity in homogenates of the retina.” A comprehensive literature examination was done in 2016 on the renin-angiotensin system (RAS) in the eye retrieved 180 publications since 1977. That many studies and nearly as many on the kallikrein-kinin system (KKS) show a strong interest in developing new medications for ophthalmology.
Diabetic retinopathy (DR) exhibit increased permeability of retinal vessels, leakage across the blood-retinal barrier and edema. Diabetic retinopathy is one of the leading causes of blindness; it can be the major cause of blindness in juvenile diabetics. Medications that block the RAS, taken orally, appear to reduce the risk of retinal microvascular complications. ACE inhibitors have a higher efficacy than angiotensin blockers (Table 1). This indicates that the ACE inhibition probably influences the KKS, as well. Kallikrein cleaves VEGF and stabilizes retinal vascular permeability and inhibits retinal neovascularization. This observation suggests that increased production of tissue kallikrein might be effective in treating diabetic retinopathy and other ocular diseases with increased VEGF production, diabetic neovascular age-related macular degeneration, diabetic macular edema, and macular edema due to retinal vein occlusion.
| ACE inhibitors | ARBs (AT1 blocking agents)‡ |
| benazepril (Lotensin) | candesartan (Atacand) |
| captopril | eprosartan (Teveten) |
| enalapril (Vasotec, Epaned) | irbesartan (Avapro) |
| lisinopril (Prinivil, Zestril, Qbrelis) | losartan (Cozaar) |
| quinapril (Accupril) | valsartan (Diovan, Prexxartan) |
| ramipril (Altace) |
Table 1. Generic and brand names for ACE inhibitors and angiotensin II receptor blockers. There are 12 different ACE inhibitors is clinical usage. A list of the ACE inhibitors that are available in the United States includes 10 medications. ‡A list of ARBs that are available in the US includes 8 medications.
Diabetic macular edema (DME) is characterized by the accumulation of fluid from the blood resulting in changes in the optical properties of the macular visual acuity. It can be either the non-proliferative or proliferative type. Despite the success of anti-VEGF treatment, a significant number of patients with DME angiogenesis did not respond to the treatment. Targeting the KKS could be promising, especially in patients who do not respond to anti-VEGF therapy for DR and DME.
Patients with age-related macular degeneration (AMD) could be classified as having early, intermediate, and late stage disease. Late stage disease may be distinguished as either wet (neovascular) or dry AMD. The wet form of AMD is often successfully treated with VEGF inhibitors. For dry AMD there is no current successful treatment to restore lost vision. Supplementation with antioxidant vitamins C and E, lutein, zeaxanthin, and zink (AREDS or AREDS2) may only reduce the progression in advanced AMD. There are some indications that RAS inhibition (AT1 receptors) might be effective for treating dry AMD.
Increased intraocular pressure (IOP) is the most important risk factor for the development of glaucoma, a neurodegenerative disease that frequently causes blindness. IOP is generated and maintained at approximately 16 mmHg. The aqueous humor within the eye is a precisely regulated balance of production and drainage. The ciliary body processes secret aqueous humor from the blood. From the posterior chamber, aqueous humor flows around the lens into the anterior chamber to drainage pathways at the angle of the anterior chamber.
The autonomic nervous system and other factors, including the role of the local RAS, play important role in the regulation of intraocular pressure. Therefore, the orally active ACE inhibitor captopril and the AT1-receptor blocker losartan lower intraocular pressure in both glaucoma patients and normal individuals. There are some findings that KKS may contribute to the reduction of aqueous outflow.
Renin-angiotensin and kallikrein-kinin systems are complex multi-protein systems present in tissues and plasma. Components of both systems are located in vascular and extravascular compartments. Although their role in physiological and pathological ocular conditions is not completely clear, numerous studies show their involvement in glaucoma, uveitis, diabetic retinopathy, diabetic macular edema, and age-related macular degeneration. Many observations indicate that local or oral administration of RAS and KKS-relevant drugs, perhaps in combined therapies could be used for the treatment of glaucoma.
Although anti-VEGF agents are effective in many patients with diabetic retinopathy and diabetic macular edema, the necessity for injection into the vitreous poses an increased risk of adverse effects. Therefore, for these and other ocular diseases, including glaucoma, and age-related macular degeneration better options are warranted. These could include stem cell and gene therapy, especially in the earlier stage of ocular diseases. Since it has been shown that renin-angiotensin inhibitors used orally slightly reduce progression and increase regression of diabetic retinopathy both in hypertensive and normotensive patients, there is hope that the road exists toward the ideal (oral) way of treatment of several ocular diseases which are the greatest threat to vision.
These findings are described in the article entitled Four decades of ocular renin-angiotensin and kallikrein-kinin systems (1977-2017), recently published in the journal Experimental Eye Research. This work was conducted by Rajko Igić from the Stroger Hospital of Cook County, University of Banjaluka, and the Academy of Arts and Sciences, Republic of Srpska.









