
Published by Neil Bailey, Kate Hoy, and Paul Fitzgerald
Monash Alfred Psychiatry Research Centre, Monash University Central Clinical School
These findings are described in the article entitled Differentiating responders and non-responders to rTMS treatment for depression after one week using resting EEG connectivity measures, recently published in the Journal of Affective Disorders (Journal of Affective Disorders 242 (2019) 68-79). This work was conducted by NW Bailey, KE Hoy, NC Rogasch, RH Thomson, S McQueen, D Elliot, CM Sullivan, and BD Fulcher from Monash University, ZJ Daskalakis from the University of Toronto, and PB Fitzgerald from Monash University and Epworth Healthcare.
Depression rates are on the rise, and with over 300 million people affected worldwide, depression is now the leading cause of disability. Antidepressant medication does not work for ~45% of people, so new treatments have been developed.
One of these new treatments is repetitive transcranial magnetic stimulation (rTMS). This treatment applies strong magnetic fields to the prefrontal cortex (an area that is underactive in depression). Because magnetic and electrical forces are linked, the magnetic field generates electrical currents in the underlying brain regions, stimulating neurons to fire. Daily rTMS treatments over the course of 5-8 weeks is able to alter brain activity (probably through neuroplastic change – Gersner et al. 2011) and improves depression in ~30% of patients (patients who typically have not responded to multiple antidepressant medications).
While this treatment alternative is great news for patients with depression that hasn’t responded to other treatments, the requirement for daily treatments over 5-8 weeks poses a considerable burden (to patients who sometimes struggle to get out of bed or leave the house). As such, the ability to predict who is likely to respond to the treatment would significantly improve patient care.
To address this problem, we performed electroencephalography (EEG) brain scans on 50 patients with treatment-resistant depression, both before they started rTMS treatment and after one week of treatment. We performed these scans while patients were resting and while they were performing a working memory task. Working memory is the ability to hold and manipulate information in the mind for a short period and is commonly disrupted in depression (as well as other cognitive functions). We compared responders and non-responders across a number of measures of brain activity. These measures included the strength of theta waves in the prefrontal cortex (a marker of attention) and the strength of connectivity between different brain regions (a marker of brain network function). We also submitted these (and other) measures of brain activity (as well as mood and working memory performance measures) to a rigorously controlled machine learning algorithm. This algorithm determined how effectively the measures might be able to predict who will respond to the treatment.
The study resulted in a relatively low response rate to treatment, with only 12 responders out of 50. However, these responders showed different brain activity compared to the non-responders at both the baseline and after one week of treatment. Responders showed stronger theta waves in the prefrontal cortex both during rest and during the working memory task, and stronger connectivity between brain regions during the working memory task. This consistent difference between responders and non-responders at both baseline and after one week of treatment suggests the measures marked a trait difference in brain activity between the two groups (rather than a change in brain activity as a result of the treatment). Responders also showed improved mood in the first week, and improved working memory performance.
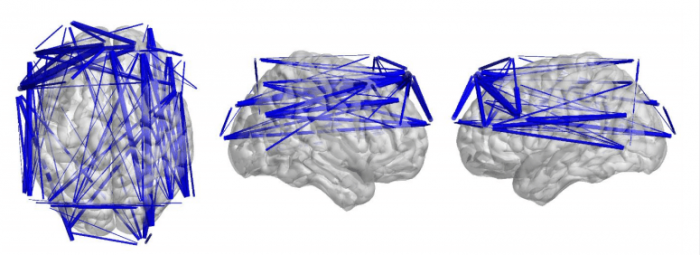
Figure 1 – Responders to rTMS treatment for depression showed significantly more theta connectivity than non-responders. Blue lines represent connections between EEG electrodes with higher theta connectivity in responders than non-responders. Image courtesy Neil Bailey.
These differences between responders and non-responders suggest there is potential to predict whether it will helpful for individual patients to continue treatment. So how did the machine learning algorithm fare at predicting the responders (using the baseline and week one brain activity, mood and working memory performance measures)? For the working memory brain scans, machine learning was highly successful at separating responders and non-responders, with a sensitivity rate of 90% (sensitivity is the ability to correctly identify responders) and a specificity rate of 92% (specificity is the ability to correctly identify non-responders). Rates for the resting brain scans were slightly lower, but still high enough to be clinically useful (with sensitivity of 84% and specificity of 89%). It should be noted that the machine learning algorithm included cross-validation (to control for over-fitting), controls for unbalanced sample sizes between the groups, and permutation testing to confirm results were not due to random chance.
If these results replicate with an independent sample (research which is currently underway), we’ll have a method to significantly reduce unnecessary burdens to patients posed by unsuccessful rTMS treatments for depression. These methods might also be applicable to other depression treatments, helping to lead to personalized recommendations for the most effective treatment and optimization depression treatment effectiveness.
At this stage, it isn’t clear whether non-responders to rTMS might respond better to another type of treatment. If they don’t, then prediction methods like those described here pose an ethical dilemma – should treatments that will probably be ineffective still be applied when there aren’t any better alternatives? rTMS has few side effects and associated risks. So even if a response is unlikely, it may still be worth trying rTMS treatment if antidepressants haven’t worked. As such, response prediction may be most useful for giving patients more information about the likelihood of response, rather than for selecting probable non-responders and not offering them rTMS treatment.
Regardless of the answer to the dilemma, the best response would be to remove the need to address the dilemma. This could be achieved by developing more treatment alternatives with better success rates, in order to increase the chance that clinicians can offer an effective treatment. Given the increasing rates of depression and the fact that pharmaceutical companies are reducing investment in the development of new antidepressants, funding for research into innovative mental health treatments is more important than ever.
References:
- Bailey, N. W., Hoy, K. E., Rogasch, N. C., Thomson, R. H., McQueen, S., Elliot, D., … & Fitzgerald, P. B. (2018). Responders to rTMS for depression show increased fronto-midline theta and theta connectivity compared to non-responders. Brain stimulation, 11(1), 190-203.
- Bailey, N. W., Hoy, K. E., Rogasch, N. C., Thomson, R. H., McQueen, S., Elliot, D., … & Fitzgerald, P. B. (2019). Differentiating responders and non-responders to rTMS treatment for depression after one week using resting EEG connectivity measures. Journal of affective disorders, 242, 68-79.
- Gersner, R., Kravetz, E., Feil, J., Pell, G., & Zangen, A. (2011). Long-term effects of repetitive transcranial magnetic stimulation on markers for neuroplasticity: differential outcomes in anesthetized and awake animals. Journal of Neuroscience, 31(20), 7521-7526.









